The most effective treatment for chlamydia. Chlamydia: symptoms, diagnosis, treatment regimens. Consequences of chlamydial infection for men
Chlamydia is a common sexually transmitted disease, the appearance of which is promoted by Chlamydia, a harmful microorganism that is difficult to identify and remove from the human body.
The bacterium has a complex development cycle, so treatment of the disease is carried out comprehensively.
Both sexual partners are treated for chlamydia. Medications are prescribed only by the attending physician.
Therapy methods
After diagnosis and confirmation of a sexually transmitted disease, therapy begins immediately. In order to completely cure the pathological condition, you will need to undergo a course of therapy with chlamydia tablets.
Medicines are selected taking into account the symptoms of the disease, distinctive features the patient’s body, the severity of the inflammatory process. Test results, immunograms and other studies are also taken into account.
Therapy of venereal pathology is carried out using:
- antibiotics (macrolides, tetracyclines, fluoroquinolones);
- probiotics;
- hepatoprotectors;
- antimycotics;
- immunomodulators;
- physiotherapy.
The latest medications are an essential component of the treatment of chlamydia in men and women. If there is no immune response to the introduction of microbes into the body, then not a single antibacterial medication will cure the patient.
Medicines
The course of treatment with drugs for chlamydia in women and men is 2–3 weeks, sometimes the therapy is longer. - an unusual microorganism that does not always immediately respond to the medications used.
Medicine claims that no treatment regimen for chlamydia in women will give a 100% guarantee of getting rid of the disease if it does not contain antibiotics.
For the treatment of chlamydia in women with antimicrobial drugs, 2 eradication schemes have been compiled:
- Consists of three drugs, which are two antibiotics and one proton pump drug.
- It consists of the use of 2 antibacterial agents for chlamydia, an antisecretory substance from the group of proton pump inhibitors and the drug bismuth. This treatment regimen is also called quadrotherapy.

If there is no positive result using the first-line regimen, doctors prescribe the use of quadruple therapy.
For the treatment of chlamydia, they are divided into three groups:
- macrolides;
- tetracyclines;
- fluoroquinols.
The disease is treated in courses, if necessary, take a short break, then repeat the therapy.
Macrolides
How to treat chlamydia in men and women?
Acute and chronic sexually transmitted diseases require the use of macrolide antibiotics.
Medicines contain a macrocyclic lactan ring; the ability of medicines to accumulate in the pathogen cell is of particular importance.

The medicine penetrates the pathogenic microorganism, which allows it to kill the affected cell faster and cure the disease.
Treatment of chlamydia in women with drugs of the macrolide class involves the use of the following drugs:
- The medicine is difficult to tolerate due to dyspeptic disorders. The drug is used according to one of the following regimens: 0.25 g 4 times a day or 0.5 g twice a day. Patients with severe disease are prescribed 0.5 g of Erythromycin 4 times a day. Tablets for chlamydia are taken for 10 days or 2 weeks. In case of a complicated or chronic illness, the medication is taken for longer than 2 weeks.
- Medicamycin. The medication is prescribed in a dosage of 400 mg three times a day. Duration of therapy is 2 weeks.
- Klarbakt and Vilprafen. Medicines are prescribed regardless of food intake. Clarbact is taken 0.25 g 2 times a day, the duration of therapy is the same as with previous macrolides. For prolonged course of the disease, the medication is used in the form of intravenous injections, dosage - 0.5 g/day. After two days of intravenous therapy, switch to oral administration. The total dosage of Vilprafen is 2.16 g/day, it is divided into three times, consumed every 8 hours, and treated for 1 week. The drug is allowed to be taken by pregnant women.
- taken once. Drink 0.5 g per day. Therapy lasts 10 days. Prescribed for pregnant women.
- Roxithromycin has high activity against bacteria. After using the tablets, the maximum concentration in the blood is reached after 1.5 hours. Drink Roxithromycin 0.15 g 2 times a day. Treatment of chlamydia in women with the drug lasts 8–22 days. Recommended during pregnancy.
When selecting antibacterial medications, factors that determine the sensitivity of the pathogen to the selected drug are taken into account.
Macrolide group drugs are selected in the same way.

Tetracyclines
Pills developed against male and female female disease, are taken according to a unified scheme established by the World Health Organization:
- Tetracycline. The dosage of the medication is 2 g/day. The total amount is divided into 4 times, taken after meals. Duration of treatment - 2 weeks.
- Doxycycline take 100 mg twice a day. The medicine is taken for 1–2 weeks. Due to the use of low doses of Doxycycline, doctors give it greater preference.
Doxycycline can be replaced with Dorix, Vibramycin, Vibra-Tabs.
Fluoroquinolones
Clinical trials have shown that drugs in this group are inferior in effectiveness to macrolides and tetracyclines.

Fluoroquinolones are rarely prescribed, only if other antibacterial medications have not helped, cause severe side effects or there are contraindications to their use.
How to treat chlamydia in men and women?

Therapy for venereal disease, if necessary, is carried out using the following fluoroquinolones:
- Take 1 week, dosage - 600 mg daily. The total dose is divided into 2 times.
- prescribed 0.4 g 2 times/day. Duration of use is 1 week; in severe cases, therapy lasts up to 10 days.
- Lomefloxacin take once 0.4 g/day. The patient claims that they were treated with it for 10 days. Doctors extend Lomefloxacin therapy if 10 days is not enough.
- Tsiprinol take 0.5 g twice a day. The disease can be cured in 1 week.
Fluoroquinolones are classified as reserve drugs. In any case, the patient will first be prescribed macrolides or tetracyclines.
Probiotics, hepatoprotectors and antimycotics
Antibacterial drugs negatively affect the intestinal microflora and liver. Macrolides, fluoroquinolones, tetracyclines disrupt the functioning of these organs.
Hepatoprotectors are prescribed to protect the liver, and probiotics are prescribed to restore intestinal microflora.

Antifungal medications prevent the development of candidiasis in women, which can occur during long-term use of antibacterial medications.
Table 1. Hepatoprotective, probiotic and antimycotic drugs for chlamydia and the scheme of their use:
|
Group |
Drug name |
Dosage regimen |
|
Probiotics |
Bifadumbacterin forte (capsules) |
2 capsules 2–3 times a day for 5–7 days |
|
2 capsules 3 times/day after meals for a week |
||
|
Lactobacterin |
5 doses 2–3 times a day, 1 dose - the contents of one bottle dissolved in 5 ml of water |
|
|
Bifiform |
2–3 capsules per day for 10–21 days |
|
|
Hepatoprotectors |
take 1-2 tablets before meals 3 times a day for 3 months |
|
|
Phosphogliv |
take 2 capsules three times a day with meals |
|
|
2 capsules 3 times/day |
||
| Antimycotics |
Fluconazole |
50–400 mg 1 time per day for the prevention of candidiasis (dosage depends on the patient’s weight) |
|
Nystatin |
500,000 units 3–4 times a day or 250,000 units 6–6 times a day |
|
|
Itraconazole |
0.2 g twice daily |
Before using medications, you should ask your doctor for permission. Self-medication is unacceptable; it can harm your health.
Immunomodulators
The use of immunostimulating tablets against chlamydia is mandatory for men and women. Medicines are part of the complex treatment of an infectious disease.
The disease suppresses the immune system of a sick person; without immunomodulating medications, it is not possible to cure the disease.
For the treatment of sexually transmitted pathology, medications from the group of recombinant interferons are used.

Table 2. Immunomodulatory drugs for patients with chlamydia:
|
Name of medicines |
Frequency of application, dosage |
|
Polyoxidonium |
0.006 g intramuscularly, administered every other day |
|
Reaferon |
2 weeks intramuscularly 1 ml |
|
Interlock |
500 IU intramuscularly for 2 weeks |
|
0.25 g intramuscularly No. 3, used daily during exacerbations, after acute symptoms subside after 24 hours |
|
| Ridostin |
8 mg intramuscularly daily during exacerbation of pathology, 48 hours after the acute period has passed |
|
0.25 g/day for two days during relapse, after 125 mg every other day – one month |
|
|
Cycloferon |
10 days intramuscularly 200 mg |
The drug Viferon is antiviral and immunomodulatory. It is enough to undergo 1 course of treatment with this medication. It is a suppository and is approved for pregnant women.
Women can be prescribed the following drugs intended to correct vaginal microflora: Alfaferon, Interferon alpha, Acylact, Genferon, Hexicon.
Mode of application
For the treatment of sexually transmitted pathology, doctors offer several methods of use medicines who have been working for more than one year.

Treatment of chlamydia in women and men with drugs - scheme No. 1:
- Antibacterial agents: Klarbakt, Sumamed.
- Hepatoprotectors: Essentiale Forte.
- Probiotics: Linex.
- Antiseptics for topical use: Aquazan, Miramistin, Hydrogen peroxide, Chlorhexidine, Betadine.
The duration of treatment is at least 21 days.
The second treatment regimen for the disease in men and women involves the use of antibacterial drugs, one of which is a fluoroquinolone, the second is a medication from the tetracycline group. Medicines are combined with Enzyme Complex Plus. The duration of therapy is 2 weeks and 1 day.
Treatment also includes a multivitamin complex and agents to stimulate digestion.
Chronic therapy
Some patients ask: “I am being treated for chronic chlamydia according to the treatment regimen for the acute course of the disease. Is it correct?".
Treatment of the chronic form of chlamydia involves a slightly different approach, it is slightly different from the treatment of the acute form. The treatment regimen depends on the degree clinical manifestations, combinations of different bacterial infections.

Table 3. Treatment of chronic chlamydia in men and women:
|
Drug name |
Application diagram |
|
Injections of Neovir or Cycloferon |
Neovir is used every other day for 2 weeks, 250 mg intramuscularly. Cycloferon daily for 10 days, intramuscularly 200 mg. |
|
Take 3 million IU 3 times a day. Start using after the third intramuscular injection of Cycloferon. |
|
|
Duflucan |
1 capsule after 1 or 2 weeks of therapy with the main antibacterial drug. |
|
Vitamin complexes |
Vitamin E - 1 tablet 2 times a day for 14 days. Ascorbic acid - 3 tablets 3 times a day, duration of use is 2 weeks. |

To treat the chronic type of chlamydia, physiotherapeutic procedures are used, these include:
- ultrasound therapy;
- laser phoresis;
- electrophoresis;
- UFOK.
These treatment methods are contraindicated during pregnancy.
Physiotherapy is prescribed only for chronic disease.
Treatment of chlamydia will be effective if the doctor has prescribed medications with high anti-chlamydial activity.
After completing the course of therapy, the patient should be re-tested for culture. Only after receiving the results of the last culture can we confidently say that chlamydia has been cured.
More than 7% of women around the world are carriers of chlamydia. Most often, chlamydia affects the genitourinary system of young women. And untimely treatment of chlamydia in women can lead to infertility or premature termination of pregnancy, which is a social problem for all of humanity.
The danger of chlamydia lies in the ability of these microorganisms to affect not only the mucous membranes of the internal genital organs, but also have a detrimental effect on the mucous membrane of the respiratory tract, the cardiovascular system, affecting the heart muscle and blood vessels. Teeth and joints are susceptible to the negative influence of chlamydia, and the process of destruction is almost asymptomatic.
Since chlamydia is a sexually transmitted disease, treatment of chlamydia in women must be carried out under the close supervision of the attending physician.
Both partners must undergo therapy. Do not self-medicate, as chlamydia is highly resistant to many medications.
- Chlamydia has the ability to quickly infect healthy cells, multiplying inside the cell from 2 to 3 days.
- Microorganisms show sensitivity to antibacterial drugs only during the reproduction period. Chlamydia is also highly resistant to drugs, which makes the treatment process much more difficult.
- Chlamydia is quite difficult to diagnose when inoculating biomaterial on a nutrient medium. And the absence of pronounced symptoms leads to progression of the disease.
- These microorganisms are resistant to external adverse conditions, showing activity at low and high temperatures.
- Chlamydia remains active in the external environment for up to 3 weeks.
- Damage to the body is expressed in the manifestation of such pathological conditions as proctitis, conjunctivitis, urogenital chlamydia, paratrachoma, acute respiratory infections, pneumonia and bronchial asthma.

Routes of infection
Timely detection of the disease and identification of routes of infection with chlamydia helps the attending physician prescribe the correct treatment. The most common route of infection is sexual intercourse with an infected partner. The disease does not necessarily manifest itself in the near future. Medical data show that the first signs of the disease can be noticed after 2-3 weeks, and in some cases, chlamydia can remain dormant in the body for up to 1 year.
Infection occurs in the following cases:
- Sexual contact with a “carrier” of infection. Infection occurs not only through traditional contact, but also during oral or anal sex. Getting on the walls of the vagina, chlamydia provokes the development of an inflammatory process that intensively affects the fallopian tubes, which subsequently leads to the occurrence of ( main reason infertility). The lesion extends to the urethra and manifests itself in the form of cystitis.
- Infection of a newborn during passage through the birth canal. Chlamydia affects the fragile body of a baby, localizing on the mucous membrane of the eyes or respiratory tract, which is expressed in the form of chlamydial conjunctivitis and pneumonia.
- Infection due to use general subjects living with an infected person. There is no official evidence of this theory of chlamydia infection, however, many experts note the possibility of infection as a result of using shared towels, clothes, underwear, and dishes. In some cases, infection has been recorded even through a handshake.
- Chlamydia, which causes chlamydial pneumonia, is transmitted by airborne droplets. This method of infection is quite rare.
It is important! A weakened body is most susceptible to infection with chlamydia. Only 15% of women who take vitamin-mineral complexes and follow the rules of a healthy lifestyle become infected.
How does chlamydia manifest in women?
The first signs of damage to a woman’s body by chlamydia appear 14 days after infection. The following changes occur in the body:
- Chlamydia enters the mucous membrane of the vagina, mouth, and eyes.
- Microorganisms penetrate the cell and multiply intensively. The duration of this period is 24-48 hours.
- The affected cell dies, which leads to the spread of microorganisms outside the cellular space and infection of healthy cells. This process is expressed in the form of inflammation.
The first signs of chlamydia in women are the following:
- vaginal discharge of mucus yellow color, which has a sharp specific unpleasant odor;
- the appearance of burning or itching, which intensifies during urination;
- general weakening of the body;
- increase in body temperature within 37-37.5C;
- the occurrence of pain in the lower abdomen.
The above symptoms may not appear at all. In 60% of patients, chlamydia is completely asymptomatic. The latent inflammatory process enters the chronic stage of chlamydia, which provokes the development of the following diseases:
- Chlamydia colpitis - occurs as a result of impaired self-cleaning of the vagina. The disease manifests itself in the form of inflammation. The most susceptible to this pathology are women who have the following abnormalities: decreased endocrine function of the ovaries, prolapse of the vaginal walls, and pathologies of the uterus. The disease is accompanied by copious vaginal discharge, swelling and redness of the external and internal genital organs. Sometimes there is a feeling of heaviness in the lower abdomen.
- Inflammation of the cervix (cervicitis). The risk group includes patients who have been diagnosed with ruptures of the cervix and perineum after childbirth, or irritation of the cervix with contraceptives. The disease has severe symptoms - pain in the lower abdomen, purulent discharge accompanied by itching and burning. The cervical mucosa becomes swollen.
- Salpingoophoritis is an infection of the fallopian tubes and ovaries. The disease is characterized by increased tone of the lower abdomen, which is accompanied by severe pain. The process of urination is disrupted and becomes painful. The inflammation process causes increased body temperature, headaches and muscle pain, weakness and psychological depression.
In some cases, specialists diagnose endometritis (inflammation of the inner mucous layer of the uterus) and salpingitis (inflammatory damage to the fallopian tubes). To avoid the risk of progression of inflammation caused by chlamydia, it is necessary to regularly undergo diagnostic procedures in medical institutions.

Diagnostic methods
The constant progression of medical diagnostic methods makes it possible to accurately determine the type of chlamydia that causes this pathology. Modern laboratory diagnostics include the following methods for identifying harmful microorganisms for a woman’s body:
- Express tests. Method for home diagnosis of chlamydia. The sensitivity of the test does not exceed 50%, so completely relying on this method is not recommended. As a result of chlamydia entering the sensitive strip, the test turns red. Positive result is expressed by the coloring of two test strips.
- Smear or microscopy. The biomaterial is scraped from the walls of the vagina, cervix or urethral opening. This method is often used, but the maximum sensitivity for detecting chlamydia is 30%. Using microscopy, an inflammatory process can be detected, which indicates the presence of pathogenic microorganisms.
- RIF (immune fluorescence reaction). The method is based on staining chlamydia with a special reagent. The sensitivity of the method reaches 70%, but this analysis method can only be performed by a highly professional specialist, which is a significant limitation in its use.
- Serological methods. The method is based on the binding of special antibodies to chlamydia. Serological methods are not widely used due to the increased likelihood of a false-positive result.
- Linked immunosorbent assay. A method of detecting not chlamydia itself, but antibodies that are produced by the body as a result of infection. The sensitivity of the method reaches 80%. Popularity this analysis received not only due to the effective detection of chlamydia, but also as a result of the ability to determine the degree of the inflammatory process and the nature of its progression.
- . The biomaterial is sown on a nutrient medium, which is sensitive only to chlamydia. The advantage of the method is the ability to select an effective antibiotic by targeting the identified chlamydia.
- Ultrasound – reveals pathological changes in internal organs as a result of the vital activity of chlamydia in a woman’s body.
Effective treatment of chlamydia in women
The disease cannot be treated independently, especially in the chronic stage of chlamydia in women. Only a complex effect on the body of specially selected medicines allows you to cure the pathology and avoid relapse.
Complex treatment consists of using the following groups of medications:
- broad and narrow spectrum antibiotics;
- immunomodulators and immunostimulants;
- multivitamin and mineral complexes;
- local antimicrobial drugs that exhibit regenerative and local anesthetic effects;
- auxiliary drugs that help reduce the negative effects of antibiotics on gastrointestinal tract and liver – enzymatic preparations, hepatoprotectors, bacteriophages.

Antibiotic therapy
Experts have identified the most effective antibiotics in the treatment of chlamydia:
- Macrolides: Azithromycin and its analogues (Sumamed, Azivok, Azitrox, Hemomycin), Josamycin, Clarithromycin (Klacid, Romiclar, Fromilid).
- Tetracyclines: (Unidox Solutab, Xedocin).
- Fluoroquinolones: Ofloxacin, Levofloxacin, Ciprofloxacin, Lomefloxacin, etc.
It is important! The necessary antibiotic is prescribed by the attending physician. If the drug does not show effectiveness, then it is necessary to inform a specialist about this so that the drug can be replaced.
The most effective drugs for the treatment of chlamydia in women are Azithromycin and Josamycin.
Immune boosters
Stimulating the production of antibodies and increasing the body's resistance to pathogenic infection is achieved through the use of drugs such as Polyoxidonium and Timalin. In addition to strengthening the body’s protective function, these drugs effectively remove toxins that chlamydia releases during its life.
Multivitamins and mineral complexes
Multivitamin preparations not only help strengthen the immune system, but also prevent chlamydia and other diseases caused by pathogenic fungi or bacteria. The pharmaceutical market offers a wide range of vitamin preparations for the treatment of chlamydia in women:
- Supradin;
- Complivit;
- Vitrum;
- Hexavit;
- Alphabet.
It is important! To improve absorption, take vitamin complexes Recommended only during meals.

Local preparations
To effectively treat chlamydia in women, eliminate itching and burning in the vagina, to eliminate infection on the walls of the mucous membrane, doctors prescribe drugs in the form of suppositories, vaginal tablets, tampons or in the form of a cream (gel). The following drugs have antimicrobial, local anesthetic, wound healing and immunostimulating effects:
- Vitaferon (suppositories);
- Hexicon (suppositories);
- (tampons);
- Propolis (tampons);
- Galavit (suppositories);
- Metrogyl (gel).
It is important! Vaginal suppositories and tablets should be used at night, taking a horizontal position of the body.
Treatment regimens for chlamydia in women
The treatment regimen for chlamydia is based on the use of antibacterial drugs and depends on the degree of progression of the disease. Special attention The doctor pays attention to concomitant pathologies that aggravate the course of chlamydia.
The specialist may prescribe the following types of antibiotic therapy:
- Monotherapy is the use of one antibiotic. Azithromycin or Josamycin and their full analogues are usually prescribed as monotherapy.
- Combination therapy is the use of several antibiotics simultaneously to improve the pharmacological effect.
Basic treatment regimens
Take Azithromycin 0.5g. 2 tablets (capsules) once a day. The duration of therapy is 7 days. After completing the course, a diagnosis is carried out that confirms or refutes the effectiveness of the treatment.
100 mg of Doxycycline should be taken 2 times a day. Duration of therapy – 7 days.
Secondary treatment regimens
The antibiotic Erythromycin should be taken 500 mg. every six hours. Duration of admission is a week.
Ofloxacin 0.3 g taken twice a day. The duration of therapy is at least 7 days.
Attention! These treatment regimens do not include drugs such as immunomodulators, hepatoprotectors, vitamin complexes and local agents. The doctor selects the name of the drugs and dosage individually depending on the patient’s condition.

Physiotherapy
Physiotherapy procedures have become widespread in the treatment of chlamydia in women, which effectively destroy chlamydia, help improve immunity and eliminate pain syndrome. Such procedures include:
- Ultrasound irradiation helps accelerate regenerative processes in the body, relieves inflammation and enhances the protective function of the immune system.
- Magnetic therapy – eliminates pain, reduces swelling of mucous membranes, slows down inflammatory processes.
- Electrophoresis - promotes vasodilation, relieving inflammation and reducing pain.
Treatment of chlamydia during pregnancy
The treatment of chlamydia during pregnancy should be approached with all responsibility, following all the recommendations of the attending physician. Because of negative influence antibiotics on the fetus, the duration of antibiotic therapy is minimized, which is 2 days. If infection is detected on early stage, then experts insist only on local treatment of the disease. It is prohibited to treat chlamydia in early pregnancy (up to 14 weeks).
It is important! During pregnancy, it is prohibited to take tetracycline antibiotics!
The safest antibiotics during pregnancy:
- Erythromycin;
- Ofloxacin;
- Amoxicillin;
- Josamycin.
The dosage of antibiotics and the frequency of use are determined by the attending physician.
Possible consequences of chlamydia
Untimely treatment and negligent attitude towards one’s health leads to the spread of infection and the progression of the inflammatory process to nearby organs and tissues. Experts have recorded the following pathological conditions:
- – leads to infertility and risk of development.
- Inflammation of the inner lining of the uterus - provokes infertility, the inability to fully bear a fetus (the likelihood of premature birth).
- Inflammation cervical canal– provokes the proliferation of atypical cells, which contributes to the development of a cancerous tumor.
- Reiter's syndrome - is expressed in the manifestation of arthritis, conjunctivitis and urethritis.
Chlamydia contributes to the disorder reproductive function women. Problems that arise due to chlamydia include:
- inability to fertilize, which occurs as a result of pathological changes in the fallopian tubes;
- fetal development in the fallopian tube (ectopic pregnancy);
- inability of the fertilized egg to attach to the uterus;
- "habitual miscarriage" - spontaneous termination of pregnancy more than three times contract;
- complications during childbirth, which is expressed in rupture of the uterine wall (due to increased tissue scarring).

Consequences of chlamydia for a newborn
- ophthalmochlamydia – manifests itself in the form of conjunctivitis;
- pneumonia;
- encephalopathy;
- Fitz-Hugh syndrome.
Disease prevention
It is important! The use of condoms does not guarantee 100% safety. The probability of becoming infected with chlamydia during sexual intercourse with a condom is 60%.
Infection with chlamydia exposes a woman's body to great danger. During long-term treatment, the patient feels not only physical, but also psycho-emotional discomfort. To avoid pathological changes and the negative effects of drugs on the body, the following rules should be followed:
- Engage in sexual intimacy only with trusted partners, using barrier contraceptives. Completely eliminate casual sex.
- Do not use other people's personal hygiene products.
- After visiting public places (toilet, swimming pool, bathhouse), it is necessary to treat the mucous membranes, as well as the skin of the hands and face with antiseptic drugs (for example, Miramistin or Chlorhexidine).
- Regularly undergo examination by a gynecologist (at least 4 times a year).
- It is necessary to be vigilant and immediately consult a doctor at the first signs of an inflammatory process.
Choose your sexual partners wisely, strengthen your immune system, engage in physical activity and be healthy!
37 034
Features of the treatment of chlamydia.
- The sooner it starts chlamydia treatment, the more effective it is.
- It is imperative that all sexual partners of the patient be examined and, if chlamydia is detected, treated (even in the absence of symptoms).
- With inadequate antibiotic therapy for chlamydia, the disease may progress to a chronic stage with the formation of antibiotic-resistant L-forms.
- There is no single treatment regimen for chlamydia. Antibiotic therapy is mandatory. And the use of immunomodulators, enzymes, hepatoprotectors and other drugs is considered individually.
- Good nutrition and a healthy lifestyle are essential for recovery. During the treatment period, it is not recommended to have sex, and drinking alcohol is strictly prohibited. It is necessary to temporarily avoid spicy food. You should also refrain from excessive physical activity.
In the treatment of chlamydia, 3 main groups of drugs are used.
- Antibiotics: tetracyclines, macrolides, fluoroquinolones.
- Immunomodulatory drugs.
- Systemic enzyme therapy drugs.
1. Antibacterial drugs.
When prescribing antibiotics for chlamydia, the following circumstances must be taken into account:
Today, in the treatment of chlamydia, it is most rational to use 3 groups of antibiotics: tetracyclines, macrolides, fluoroquinolones.
a) Tetracyclines
Doxycycline (vibramycin, unidox solutab). The first dose is 0.2 g, then for two weeks 2 times a day, 0.1 g. The course should be 2.5 - 4 g of the drug. Disadvantages: side effects: nausea and vomiting, rarely - impaired bone formation, defects in tooth enamel. The use of tetracyclines is contraindicated during pregnancy and breastfeeding and in children under 14 years of age. Unidox Solutab and vibramycin are better tolerated than doxycycline.
b) Macrolides.
Macrolides are the safest antibiotics. They have a minimum of side effects and are well tolerated. All of them are active against treponema pallidum, mycoplasma, ureaplasma, gonococcus, which allows them to be used for mixed infections. The effectiveness of macrolides, according to experts, reaches 91-97%.
- Erythromycin. Its effectiveness is 85% - 95%. Disadvantages: severe dyspeptic disorders and the need for 4 doses. Use 500 mg 4 times a day for 2 weeks.
- Vilprafen (josamycin). It is considered the most effective in most cases and the safest. For a fresh form of chlamydia - 500 mg 2 times a day for 2 weeks. For chronic - 500 mg 3 times a day for 4 weeks. The initial dose is 1 g once. Resistance to josamycin develops less frequently than to other antibiotics from the macrolide group.
- Rovamycin (spiromycin). Prescribed 3 million units 3 times a day for 2 weeks.
- Rulid (roxithromycin). Use 150 mg 2 times a day for 2 weeks.
- Macropen (midecamycin). Prescribed 400 mg 3 times a day for 2 weeks.
- Sumamed (azithromycin). Prescribed according to the following scheme: the first day 1 g once, then 0.5 g for 7 days. The course is designed to take 3 g of the drug. Recently, resistance of chlamydia to sumamed has been noted. Therefore, you can replace it with Hemomycin, the active ingredient of which is also azithromycin.
- Klacid (clarithromycin). Take 250 mg twice daily for 2-3 weeks.
During pregnancy, it is allowed to use erythromycin 500 mg 4 times a day for 2 weeks or rovamycin 3 million units 3 times a day for 2 weeks.
c) Fluoroquinolones.
They are less effective than macrolides and tetracyclines. However, they are active against gonococcus, mycoplasma, and gardnerella. Contraindicated during pregnancy, as well as in children under 14 years of age. They have a significant number of side effects.
- Ofloxacin (zanocin, tarivid) 200 mg after meals 2 times a day for 10 days.
- Abactal (pefloxacin). Fresh and uncomplicated chlamydia - 400 mg twice a day for 1 week. Chronic form – 10-12 days.
- Maxaquin (lomefloxacin). For a fresh, uncomplicated form - 400 mg once a day for a week. For chronic use - 400-600 mg/day, course 28 days.
- Tsiprobay, Tsiprolet, Tsifran (ciprofloxacin). For fresh, uncomplicated forms of chlamydia, 500 mg is taken at the first dose, subsequent doses - 250 mg twice a day for 7 days. For chronic and complicated forms - 500 mg twice a day for 12 days.
2. Immunomodulatory therapy.
With chlamydial infection, suppression and changes in the state of the immune system occur, which creates the basis for the chronicity of the process. Therefore, during treatment it is necessary to act not only on the pathogen itself, using antibiotics, but also to increase the body’s resistance, strengthening the immune system. However, immunomodulators are not always used - in each specific case individually.
The following immunomodulators are used:
- Immunomax. The recommended dose for adults is 100-200 U IM 1 time/day. Course of treatment – 6 injections on days 1, 2, 3, 8, 9, 10 of treatment.
- Polyoxidonium. It is used to treat atypical forms of chlamydia in cases of impaired immunological status. Polyoxidonium increases the formation of antibodies and the body's immune resistance. Used in a course of 10 injections of 6 mg every other day.
- Erbisol. 2 injections per day: 2 ml in the morning at 8 o’clock and in the evening at 22 o’clock, course 20 days. It also protects the liver, being a hepatoprotector.
3. Systemic enzyme therapy.
Preparations for systemic enzyme therapy normalize the permeability of cell membranes in areas of inflammation. Thus, higher concentrations of antibiotics penetrate into the cell at lower doses. They enhance the effect of antibiotics, increasing their concentration in the blood serum by 20-40%. They block mechanisms that trigger allergic (including to medicinal drugs) and autoimmune reactions, accelerate the elimination of toxins, and provide decongestant and analgesic effects.
Preparations:
- Wobenzym. Prescribed 3 tablets. 3 times a day 30 minutes before meals, with a glass of water, course 2-4 weeks.
- Phlogenzyme. Prescribed 2 tablets. 3 times a day 30 minutes before meals, with a glass of water, course 2-4 weeks.
4. Hepatoprotectors.
The prescription of this group of drugs is due to the long-term use of antibiotics, which are metabolized in the liver, creating an increased load on it. Moreover, tetracyclines and fluoroquinolones are hepatotoxic and can cause liver damage. Preparations:
- Essentiale - 2 caps. 2-3 times a day with meals, course 2-4 weeks
- Karsil - 70 mg 3 times a day after meals, course 2-4 weeks
- Legalon - 70 mg 3 times a day after meals, course 2-4 weeks
5. All other groups of drugs are used individually.
If dysbacteriosis has developed, use eubiotics Bifidumbacterin, Acylact, etc.
Vitamins and antioxidants may also be prescribed.
How to make sure that you are cured?
The disappearance of clinical manifestations of chlamydia after a course of treatment is not proof that the body has gotten rid of the pathogen. Sometimes the use of antibiotics leads only to local improvement. Therefore, a month after completion of antibiotic therapy, it is necessary to conduct control tests. If chlamydia is not found, then repeated tests are carried out after a month. If after a month the tests for the presence of chlamydia are negative, only then will it be possible to talk about the effectiveness of the treatment.
The following laboratory tests are used:
- ELISA for IgA - there is no IgA during recovery.
- PCR – upon recovery, PCR is negative.
- All other methods laboratory diagnostics uninformative.
I immediately went to the KVD. They took all the tests, but the next day they said that they found nothing... I'm in shock. I went to another KVD, they didn’t find it there either, but they explained... that they take it for everything except chlamydia. Then I went to the Research Institute of Epidemiology (CED), where I was tested for all infections, where I was successfully diagnosed with chlamydia.
The immediate question is where and how to treat it if you don’t work and there is no way to waste money. I called about 15 Moscow clinics. Treatment of chlamydia from 5-15 thousand rubles, over a period of time from a week to a month (at least that’s what urologists and venereologists claimed). There is no money. I don’t know what to take. The only help here is my INTERNET, all my hope is on it. At the request “ask a question to a urologist or venereologist,” my Internet gave me many sites where you can ask a doctor a question online. Guys...what a mess this is all. Look, not one of the doctors answered you specifically...what can be treated and how, citing delusional medical ethics and a bunch of other reasons, just as illegible. People with a problem turn to doctors online, asking for help, and what in response. Come to the appointment... we won’t say in absentia... medical ethics.
ONLINE sites all over the world have been created so that a doctor can actually provide online advice to people who, for some reason, cannot go to a paid doctor or hospital. With us, everything is in “one” place. For example, this is how a face-to-face consultation differs from a correspondence consultation in my case. I have a certificate of tests confirming CHLAMYDIOSIS and nothing more. And I can also tell you the date of infection. ALL. This is enough for 90% of all doctors to prescribe a course of treatment... and there is no need to show anything, everything is already clear.
And what. To say and show this, I need to go somewhere. ABSOLUTELY NOT.
But doctors need to extract money... this is their salary. And that’s why no one says either a treatment regimen or really other answers... everything is the same... COME.
And then I began… going through torment.
I turned to a dermovenerologist for help. I was prescribed Doxycycline hydrochloride and Metronidazole... took it for a week... no changes. Then they prescribed TARIVID (ofloxacin). I took it for a week and it didn’t help. I started injecting chlorhexedine bigluconate 0.05% into the urethra for 3 minutes (as the doctor said)
It burned the entire urethra, the white discharge was replaced by a cloudy-rusty...thick...to urinate, you had to simultaneously howl in pain. Guys...this is SUCH pain...this is the second birth, probably...only for a man.
In short...I'm disappointed...heartbroken...and still having an infection.
Here I accidentally came across a urologist-venerologist from a large Moscow military hospital on the Internet. I tell him everything, and he tells me the following:
“I can prescribe a course of treatment for you right now, in absentia, and the result will be %, the maximum course is two to three weeks and there is nothing complicated about it, urogenital chlamydia is treated with the same type of drugs, only they can be called differently. These can be tetracyclines (doxycycline), macrolides (for example, azithromycin (sumamed), fluoroquinolones.
CLABAX (clarithromycin) is a leader in the treatment of chlamydial infection, 250 mg - the first 3 days, 3 times a day, then 2 times a day, every 12 hours for 14 days. Chlamydia is a harmful virus and has no easy cure. I started taking it with no hope. But, fortunately...on the 10th day I got up in the morning....and that’s it...no discharge...no symptoms.
After waiting one month, after taking the antibiotic, I was checked for infection - NO INFECTION...I'M CLEAN..like a child J.
If suddenly this drug does not help anyone, the doctor said, maybe this is the case... here is a comprehensive method of treating chlamydia, which did not respond to previous treatment.
1.Unidox – 100 mg each. 2 times a day
I was cured, I drank dietary supplement Sanaris, I bought Chinese dietary supplements in Haogang that help with chlamydia, ureaplasmosis, gardnelosis, and much more. Then I also found out that a decoction of wormwood helps. I drank it. I ate raw nettle. I also heard that it helps with such STDs. Before that, I was prescribed antibiotics, but they made me feel sick, stomach reaction, and I spent money. Then I went to haogang and bought a dietary supplement there, maybe wormwood helped, I don’t know
Mikhail, I recently found out that I have chlamydia. They prescribed a number of antibiotics and I took them. Now I have been prescribed Doxycycline and Josamecin to take for 8 weeks. I don’t know if the guy has this problem, but is it a good idea for him to take 1 drop for 10 days as a preventive measure? 2 times a day doxycycline?
Lavomax 1,2 day and then every other day. Tigeron 750 (levofloxacin) tablet 1 piece per day for 10 days, vilprafen 500. 2 tablets. In a day. 10 days. Fluconazole 150 mg 1 pc. And only with chlamydia intracellular diseases. If there is Trichomonas gardnerella, other tablets are used against them.
And the doctor may add gastroprotectors and hepatoprotectors for health reasons. Chlamydia can be treated well. If there was a course of treatment before this, there was. You have to wait a month for analysis and recovery of the body. I am a former patient and am sharing my experience. And so the doctor knows better. There are just different doctors. The main thing is to find a good doctor. Do not be ill.
If you are undertreated or cured. If the guy has junk. You will become infected again, so you and your partner will need to complete your treatment at the CVD. No options. And for prevention, taking pills is not at all correct. You are your own trash. If you get beaten, it will be difficult to heal. And health and immunity will decrease. So find a good venereologist. And not separately. Go together
Almost a month later from the moment of no contact with Venya. They took three swabs. A week later the result. Chlamydia and other things are not a serious disease. I don’t remember what it’s called, I didn’t take the test results (it was scary). I prescribed safocid 4 caps (four at once). Unidox salutab 1t2 times 14 days. I took a vacation to drink and rest. In the evening there were 4 saphocides at once. On the trail of Unidox. I started drinking the current incorrectly. When I got home I threw the sheet away. The first three doses were not 1, but 2. Then I looked that it wasn’t enough for 14 days and found a sheet. I started taking it 1 at a time. While I was drinking, the result seemed to be visible. (I took all 15d tablets) after taking it for 16 days I feel the treatment has not worked. Wait a month for tests. There’s no point in going to a fortune teller, I’ll say that it didn’t help because the syndromes remained. There are 2 weeks left before the tests. I started having problems with my stomach and won’t eat heavy foods. Nausea boils over. I can’t eat anything at all; I’m weak. (Stomach is weak; ulcers were treated 3 months ago). Fears panic attacks. What should I do? The intestines were killed during the cabbage soup campaign (I didn’t take anything for microflora, they didn’t draw it). When can I start the 2nd course? And what is better? (sorry for the harpography)
Usually there is at least a 2-4 week break between courses. If there are problems with the gastrointestinal tract, then again it is better to resolve this issue with a doctor, check for fungi and conditionally pathogenic flora. But at least switch to simple lean food: porridge, non-acidic juices (carrots and celery), stewed grated vegetables, poultry and fish. Be sure to take a test for Trichomaniasis in addition to Chlamydia (or, to be on the safe side, ask your doctor to include it in the course, since in men it is difficult to detect even with the help of PCR) In general, the patient’s task is simple to wait until the tests are taken, during which time do normal activities and eat well (simple, easily digestible food), do not self-medicate and, most importantly, cheer up - Everything will be good!
Thank you very much for the answer! Nice. Started the second course.
Levofloxacin - instructions for use, reviews, analogs and release forms (250 mg, 500 mg and 750 mg Hyleflox tablets, solution for infusion, 0.5% antibiotic eye drops) drug for the treatment of pneumonia in adults, children and pregnancy. Compound
In this article you can read the instructions for use of the drug Levofloxacin. Reviews of site visitors - consumers of this medicine, as well as the opinions of specialist doctors on the use of the antibiotic Levofloxacin in their practice are presented. We kindly ask you to actively add your reviews about the drug: whether the medicine helped or did not help get rid of the disease, what complications and side effects were observed, perhaps not stated by the manufacturer in the annotation. Analogues of Levofloxacin in the presence of existing structural analogues. Use for the treatment of pneumonia, prostatitis, chlamydia and other infections in adults, children, as well as during pregnancy and lactation. Composition and interaction of the drug with alcohol.
Levofloxacin is a synthetic broad-spectrum antibacterial drug from the group of fluoroquinolones, containing levofloxacin, the levorotatory isomer of ofloxacin, as an active substance. Levofloxacin blocks DNA gyrase, disrupts supercoiling and cross-linking of DNA breaks, inhibits DNA synthesis, and causes profound morphological changes in the cytoplasm, cell wall and membranes.
Levofloxacin is active against most strains of microorganisms (aerobic gram-positive and gram-negative, as well as anaerobic).
Other microorganisms that are sensitive to the antibiotic Levofloxacin are: Bartonella spp, Chlamydia pneumoniae, Chlamydia psittaci, Chlamydia trachomatis, Legionella pneumophila, Legionella spp, Mycobacterium spp, Mycobacterium leprae, Micobacterium tuberculosis, Mycoplasma hominis, Mycoplasma pneumoniae, Ricketsia spp, Ureaplasma urealyticum.
Levofloxacin hemihydrate + excipients.
Levofloxacin is rapidly and almost completely absorbed after oral administration. Food intake has little effect on the speed and completeness of absorption. Penetrates well into organs and tissues: lungs, bronchial mucosa, sputum, genitourinary organs, bone tissue, cerebrospinal fluid, prostate gland, polymorphonuclear leukocytes, alveolar macrophages. In the liver, a small portion is oxidized and/or deacetylated. It is excreted from the body primarily by the kidneys by glomerular filtration and tubular secretion. After oral administration, approximately 87% of the dose taken is excreted unchanged in the urine within 48 hours, less than 4% in the feces within 72 hours.
Infectious and inflammatory diseases caused by microorganisms sensitive to the drug:
- lower respiratory tract infections (exacerbation of chronic bronchitis, community-acquired pneumonia);
- ENT infections (acute sinusitis);
- urinary tract and kidney infections (including acute pyelonephritis);
- genital infections (including bacterial prostatitis);
- infections of the skin and soft tissues (festering atheromas, abscess, boils);
- intra-abdominal infections;
- tuberculosis (complex therapy of drug-resistant forms).
Film-coated tablets 250 mg, 500 mg and 750 mg (Hyleflox).
Solution for infusion 5 mg/ml.
Eye drops 0.5%.
Instructions for use and dosage
Orally, during meals or in between meals, without chewing, with a sufficient amount of liquid.
Doses are determined by the nature and severity of the infection, as well as the sensitivity of the suspected pathogen,
For acute sinusitis, once a day for a day;
For exacerbation of chronic bronchitis - from 250 to 500 mg 1 time per day for 7-10 days;
For community-acquired pneumonia, 1 or 2 times a day for 7-14 days;
For uncomplicated urinary tract and kidney infections, mg once a day for 3 days;
For complicated urinary tract and kidney infections, mg once a day for 7-10 days;
For bacterial prostatitis, mg 1 time per day for 28 days;
For infections of the skin and soft tissues, mg mg 1 or 2 times a day for 7-14 days;
Intra-abdominal infections - 250 mg 2 times a day or 500 mg 1 time a day (in combination with antibacterial drugs acting on anaerobic flora).
Tuberculosis - 500 mg orally 1-2 times a day for up to 3 months.
If liver function is impaired, no special dose adjustment is required, since levofloxacin is only slightly metabolized in the liver and is excreted primarily by the kidneys.
If you miss a dose of the drug, you should take the pill as soon as possible before the time for your next dose approaches. Then continue taking levofloxacin according to the schedule.
The duration of therapy depends on the type of disease. In all cases, treatment should be continued for 48 to 72 hours after the symptoms of the disease disappear.
- itching and redness of the skin;
- general hypersensitivity reactions (anaphylactic and anaphylactoid reactions) with symptoms such as urticaria, constriction of the bronchi and possibly severe suffocation;
- swelling of the skin and mucous membranes (for example, in the face and throat);
- sudden fall blood pressure and shock;
- increased sensitivity to solar and ultraviolet radiation;
- allergic pneumonitis;
- vasculitis;
- toxic epidermal necrolysis (Lyell's syndrome);
- exudative erythema multiforme;
- nausea, vomiting;
- diarrhea;
- loss of appetite;
- stomach ache;
- pseudomembranous colitis;
- a decrease in blood glucose concentration, which is of particular importance for patients suffering from diabetes mellitus(possible signs of hypoglycemia: increased appetite, nervousness, perspiration, trembling);
- exacerbation of porphyria in patients already suffering from this disease;
- headache;
- dizziness and/or stupor;
- drowsiness;
- sleep disorders;
- anxiety;
- shiver;
- psychotic reactions such as hallucinations and depression;
- convulsions;
- confusion;
- visual and hearing impairments;
- disturbances of taste sensitivity and smell;
- decreased tactile sensitivity;
- increased heart rate;
- joint and muscle pain;
- tendon rupture (for example, Achilles tendon);
- deterioration of kidney function up to acute renal failure;
- interstitial nephritis;
- increase in the number of eosinophils;
- decrease in the number of leukocytes;
- neutropenia, thrombocytopenia, which may be accompanied by increased bleeding;
- agranulocytosis;
- pancytopenia;
- fever.
- hypersensitivity to levofloxacin or other quinolones;
- renal failure (with creatinine clearance less than 20 ml/min - due to the impossibility of dosing this dosage form);
- epilepsy;
- tendon lesions due to previous treatment with quinolones;
- childhood and adolescence (up to 18 years);
- pregnancy and lactation period.
Use during pregnancy and breastfeeding
Contraindicated during pregnancy and lactation.
Levofloxacin should not be used to treat children and adolescents (under 18 years of age) due to the likelihood of damage to articular cartilage.
In severe pneumonia caused by pneumococci, levofloxacin may not provide an optimal therapeutic effect. Hospital-acquired infections caused by certain pathogens (P. aeruginosa) may require combination treatment.
During treatment with Levofloxacin, seizures may develop in patients with previous brain damage caused, for example, by stroke or severe trauma.
Despite the fact that photosensitivity is observed very rarely with the use of levofloxacin, in order to avoid it, patients are not recommended to be exposed to strong solar or artificial ultraviolet irradiation unnecessarily.
If pseudomembranous colitis is suspected, levofloxacin should be discontinued immediately and appropriate treatment should be initiated. In such cases, drugs that inhibit intestinal motility should not be used.
The consumption of alcohol and alcoholic beverages during treatment with Levofloxacin is prohibited.
Rarely observed with the use of the drug Levofloxacin, tendonitis (primarily inflammation of the Achilles tendon) can lead to tendon rupture. Elderly patients are more prone to tendonitis. Treatment with glucocorticosteroids appears to increase the risk of tendon rupture. If tendonitis is suspected, treatment with Levofloxacin should be stopped immediately and appropriate treatment of the affected tendon should be initiated.
Patients with glucose-6-phosphate dehydrogenase deficiency (an inherited metabolic disorder) may respond to fluoroquinolones by destroying red blood cells (hemolysis). In this regard, treatment of such patients with levofloxacin should be carried out with great caution.
Impact on the ability to drive vehicles and operate machinery
Side effects of Levofloxacin, such as dizziness or drowsiness, drowsiness and visual disturbances, may impair reactivity and ability to concentrate. This may pose a risk in situations where these abilities are particularly important (for example, when driving a car, when servicing machinery, when performing work in an unstable position).
There are reports of a pronounced decrease in the seizure threshold with the simultaneous use of quinolones and substances that can, in turn, reduce the cerebral seizure threshold. This also applies equally to the simultaneous use of quinolones and theophylline.
The effect of Levofloxacin is significantly weakened when used simultaneously with sucralfate. The same thing happens with the simultaneous use of magnesium or aluminum containing antacids, as well as iron salts. Levofloxacin should be taken at least 2 hours before or 2 hours after taking these medications. No interaction was detected with calcium carbonate.
When using vitamin K antagonists simultaneously, monitoring of the blood coagulation system is necessary.
The elimination (renal clearance) of levofloxacin is slightly slowed down by the action of cimetidine and probenecid. It should be noted that this interaction has virtually no clinical significance. However, with the simultaneous use of drugs such as probenecid and cimetidine, which block a certain excretion pathway (tubular secretion), treatment with levofloxacin should be carried out with caution. This applies primarily to patients with limited renal function.
Levofloxacin slightly increases the half-life of cyclosporine.
Taking glucocorticosteroids increases the risk of tendon rupture.
Analogues of the drug Levofloxacin
Structural analogues of the active substance:
Medical history + 2 diagrams, one helped. Help with reviews.
The symptoms are generally standard, except for the fact that at the end of urination I had white flakes coming out, like some kind of milk, along with this there was such a sting that I sat down on my butt on a hot radiator just to let a little bit pass.
Dazolic 3 pack: 1 t in the morning, in the evening.
Prostopin suppositories 1 pack
Pyrogenal - 10 injections
This is all your lifestyle, you are healthy - he answers.
Trichopolum 2t morning/2t evening - 10 days
Unidox 1t morning/1t evening - 25 days
Candles with Tambukin mud
Fluconase 1 t every 5 days
Morning boner - almost every day
Cheerfulness - appeared
WHITE FLAKES - no
There are no constant cutting pains.
Day to day the state is different, sometimes I stand for 5-6 seconds before pissing, sometimes right away, sometimes I feel a distant burning sensation, sometimes it seems that I am now completely healthy.
At night I pissat - 1/2 times, but I drink it before going to bed.
There are almost no spontaneous erections during the day.
Sometimes I don’t feel like having sex at all for 2-3 days.
I drank Tavanik even before all this started, for 14 days, it was of little use.
Now I’m thinking of finishing off the infection with a long-term regimen of macrolide + fx 4 potalinium + tetracyclines.
I don’t refer to my analyzes because... They found everything for me, and then nothing, and so many times. Now I trust tests even less than doctors; I have to rely on sensations: low libido, delay, or premature termination of sexual intercourse, slight non-periodic burning sensation during pissing. severe pain and a complete lack of libido and erection went away thanks to a 25-day course of Unidox. 2 months after that, the tests were clear, and then myco and urio plasma came out for ELISA secretion. Believe it or not, I don’t know, but it was decided to finish off the infection based on the symptoms.
0.75 g every 8 hours x 10 days
1t x 1 day x 21 days, but take 500 mg for the second week
Fluconazole 50 mg once every 5 days
There is an opinion that Vilprafen is not the best option To solve the issue of biofilms, you need to beat them with 14,15-membered macrolides. Based on this, how do you look at the idea of replacing it, for example, with Azithromycin once a day. I can’t take Clarithromycin, I’ve already taken Klacid for 28 days, so I’d try Ecositrin.
1 Antitrichomonas (Trichopol, Furomag, Cycloferon, Atrican)
2 From trash (Unidox, Sumamed, Longidaza or Lidaza 20 days, Galavit)
3 broad spectrum Abt (Avelox, etc.) plus Derinat injections.
There is an opinion that Vobezim is not the best option for solving the issue of biofilms
thanks for the reply.
won't there be a lot of anti-trichomonas drugs? and then Unidox with azitrimycin for 20 days + Avelox 21 (and I’m still thinking about 25). Taking into account 10 days of anti-trichine, my course will be 55 days. I worry about the state of the body after the course I proposed, and after this I think in general I will not remain alive.
Go to the three thread, in the last topic I posted courses from respected medical institutes)))
Forget about the EU, people come from there and we are stocked with pyrogenal (((I’m too lazy to look, but there are just a ton of clinical cases of positive therapeutic effects on pyrogenal. If it gets hard, then take short breaks between courses. Your chlamydia won’t get away from you.) ))
Why change Wobenzym to Pyrogenl? Because this is the only drug I know of that transforms a chronic disease into an acute form. As you know, the acute form is much easier to treat.
V.A. Molochkov, prof., doctor of medical sciences
Urogenital chlamydia: clinical picture, diagnosis, treatment
The treatment of urogenital chlamydia is a very complex problem. Only in case of uncomplicated fresh acute and subacute lesions of the urethra, mucous membrane of the cervical canal or rectum, one can limit oneself to etiotropic drugs (Table 1).
Oxy- and chlortetracycline 2000 mg/day for adults orally
Doxycycline (vibramycin) 200 mg/day orally
Erythromycin 2000 mg/day orally
Roxithromycin (rulid) 300 mg/day orally
Azithromycin (sumamed) mg/day orally
Spiramycin (rovamycin) 9.0 g/day 1.5 million units/day No. 12-15 orally lymphotropically
Clarithromycin (klacid, clubax) 500 mg/day orally
Ofloxacin (zanocin, etc.) mg/day orally
Lomefloxacin (Maxaquin) 800 mg/day orally
CHAPTER 1 MODERN ASPECTS OF UROGENITAL CHLAMYDIAL INFECTION
Considering the intracellular localization of C. trachomatis, treatment should use drugs that penetrate well into the cell (Lykova S. G., Khryanin A. A., 1998; Granitov V. M., 2000). According to the degree of penetration, antimicrobial drugs are conventionally divided into groups with a low degree (penicillins, cephalosporins, nitroimidazoles), a medium degree (tetracyclines, aminoglycosides, rifampicin, fluoroquinolones) and a high degree (macrolides). The main antibacterial drugs used for the treatment of UGC are tetracycline antibiotics, macrolides and fluoroquinolones (Savicheva A.M. et al., 1999; Kisina V.I., 2000; Khryanin A.A., 2001; Methodological materials for diagnosis and treatment the most common STIs and skin diseases, 2003; Molochkov V. A., Molochkov A. V., 2005; Fedotov V. P. et al., 2005; Prospects for increasing the effectiveness of treatment for CI may be associated with the introduction of a new group of antibiotics - ketolides (telithromycin, etc.) (Pavletic A. J. et al., 1999).
or roxithromycin (Rulid) 150 mg orally 2 times a day for 7 days;
fluoroquinolones: ofloxacin (300 mg orally after meals 2 times a day for 7 days or 400 mg 1 time a day for 7 days).
josamycin 500 mg orally 2 times a day for 14 days.
In addition, the following treatment regimens for urogenital chlamydia are found in the literature:
metacycline (rondomycin) - on the 1st day 600 mg, then 300 mg 3 times a day for 7-10 days;
azithromycin (sumamed, zitrolide, hemomycin, azitral) - 1st day once 1 g per day, the next 4 days 500 mg per day, course dose 3 g;
clarithromycin (clacid, clubax, fromilid) 250 mg orally 2 times a day for 7-10 days or 1 g on the first day and 0.5 g orally once a day for 4 days. One of the representatives of 14-membered semisynthetic macrolides is clarithromycin, which has high activity against C. trachomatis, superior to that of antichlamydial drugs widely used in the clinic. This antibiotic has higher penetration and the ability to accumulate in the cells of the macroorganism, including immunocompetent ones. Unlike azithromycin, clarithromycin does not create long-term subinhibitory concentrations, so the risk of developing resistance to this drug is much lower. It has been established that clarithromycin is the only uroselective macrolide with a high percentage of excretion through the kidneys. The good tolerability and safety of clarithromycin has been confirmed; adverse reactions are rare and do not require discontinuation of the drug. The drug is used in a dosage of 250 mg twice a day for a day. Clarithromycin is a first-line drug (along with the traditional doxycycline and azithromycin) for the treatment of UGC;
spiramycin IU 3 times a day for 10 days, as well as midecamycin (macropen), pristinomycin.
levofloxacin (Tavanic) 250 mg 2 times a day for 7-10 days or 500 mg 1 time a day for 10 days. Levofloxacin is more active against chlamydia and, given once daily dosing, has a higher compliance;
lomefloxacin (0.6 g 1 time per day for 7 days), pefloxacin and other fluoroquinolones for adults and children over 12 years of age.
Unidox (this is another name for doxycycline) is correct, everything else is wrong, you absolutely don’t need any of the above. You can read about the accepted international treatment regimen for chlamydia in this topic above.
Mycoplasma and ureaplasma in your case do not require any treatment at all, since it is part of your normal vaginal flora. You can read about this in the topic “Mycoplasmosis and ureaplasmosis - how bad is it?”
Obstetrician-gynecologist, ultrasound specialist, Ph.D. Borisova Alexandra;
Make an appointment by email: or by phone
From: Molodechno, Belarus
The only reliable method of diagnosing whether a person currently has chlamydia in the body or not is an analysis to determine the presence of chlamydia antigen (i.e., chlamydia itself) in the cervical canal/urethra in women and the urethra in men. To do this, they use different methods, including PCR.
They look for antibodies to chlamydia in the blood. When chlamydia enters the body, after some time antibodies are produced in the human blood. These antibodies remain in a person's blood for life. If you do not have antibodies to chlamydia in your blood, then with a very high degree of confidence we can say that you have never had chlamydia in your body before and at the moment. However, antibodies to chlamydia begin to be produced approximately 7-14 days after chlamydia enters the human body. Therefore, if we assume that chlamydia entered your body approximately 6-13 days ago, then a blood test for antibodies to chlamydia will not show anything (i.e. it will be negative). Tests to determine chlamydia itself in the cervix/urethra in women, as well as in the urethra in men, also become positive approximately a day after chlamydia enters the body. That's why it's useless to run out and do a chlamydia test the day after intimacy with a new partner.
Obstetrician-gynecologist, ultrasound specialist, Ph.D. Borisova Alexandra;
Levofloxacin for chlamydia reviews
For a long time, there have been “seasons” of exacerbation with discharge. At the end of urination there is a cloudy white sediment and a burning sensation. In the last fateful year, February 2017. There was work at heights in frosty weather. All day. About 1.5 months. I experienced a severe aggravation and began to try again to recover. This disease has been around for about 10 years. I didn’t know what it was like to have pain in the balls or, as they say, in the prostate. And I didn’t even think that I already had chronic prostatitis. It always stood properly, and spat everyone properly)))
So I took a smear test for STIs - it was clear. Afterwards, a swab on the tank is inoculated - clean. After three days with provocation, a smear from the urethra for PCR, for 6 pathogens:
Chlamydia, ureaplasma, mycoplasma, trichomonas, gardnerella and candida.
They prescribed a course that seemed weak to me:
Trichopolum 500 mg 2 times a day for 5 days.
And I don’t remember the dosage of ornidazole for 5 days.
So when I ate azithromycin it went very well. I was 99% healthy. On day 5, symptoms began to return. After stopping the course two days later there is an exacerbation and discharge like flakes:
And then, after the course, I experienced a severe exacerbation three days after finishing taking Itracon.
Urine tests for tank culture, high titers of opportunistic bacteria:
Then I was switched to suprax solutab tablets for 10 days. And after Levomac 500 mg. 10 days. (I also think it’s not enough) according to the instructions for HP you need to eat it for 28 days. Rather, they developed resistance.
Maybe this means that chlamydia is deeply embedded and can no longer be detected by PCR? But only ELISA? I’ve read many places that this is the case with chlamydia, like this infection is still the same.
The epididymal cyst is bilateral.
And I also think that it was necessary to include immunomodulators in the course.
At the moment I have been prescribed doxycycline (Unidox Solutab). I have been taking it for 11 days already, the first two doses are 200 mg loading dose, the next 100 mg. Twice a day and I take Omnic in parallel. These six months, constant chronic fatigue is especially evident after one o'clock in the afternoon. In the evening I already ate my legs and dragged them home. My work is not hard. What should you take for chlamydia, biseptol or levofloxacin? According to the sensitivity of the flora, levofloxacin is suitable according to the latest analysis. Biseptol, according to reviews, saved many (those who had already eaten all possible pills).
Chlamydia. Treatment of chlamydia
#461 Praskovya //
Knocked on the door
Divia is most likely a scam, I’m talking about treatment. In my opinion, you can retake the test for junk using the PCR method elsewhere, maybe there’s nothing to treat. :scratch: I know one unfortunate doctor who assigns diagnoses to everyone and sends them to buy medicine from his nurse, and she herself sells illegal drugs.
We were treated with one drug together with my husband, I also had suppositories + a tablet for thrush at the end of treatment. The course was 10 days.
Advertising
#462 ₪₪Girl in a chintz dress₪₪
Received a residence permit
And I know that one of my friends was also diagnosed with some diseases, in my opinion this was “it”; she was prescribed treatment, but they told him there was no need, because they didn’t detect it twice, and they allegedly argued that he had some kind of immunity to it (I’m shocked, of course, but there’s no point in deceiving the doctor. I don’t know: scratch:) and This immunity is connected with a previously cured disease in this clinic in some super way, which consisted not only of pills, but also of some daily procedures with a doctor.
What do you say? :spiteful:
#463 Divia
And I already thought the trash was back.
And congratulations to you too on your victory over this bullshit))))
#464 Divia
#465 I'm waiting, I hope
#466 Julia1987
anti-Chlamydia tr. IgA 16 titer SM. COMM. 60 - positive.
anti-Chlamydia tr. IgG 12 titer SM. COMM. 60 - positive.
Chlamydia trachomatis NOT DETECTED
Mycoplasma hominis NOT DETECTED
Ureaplasma ur.T-960 NOT DETECTED
Ureaplasma parvum NOT DETECTED
Gardnerella vaginalis NOT DETECTED
Neisseria gonorrhoeae NOT DETECTED
Trichomonas vaginalis NOT DETECTED
Mycoplasma genitalium NOT DETECTED
anti-Chlamydia tr. IgM negative
#467 Xanarrr-Bellied Doe
Where was chlamydia found?
#468 Julia1987
Although they are negative, the credits are equal, that is, 16 and 12?
#469 Saina
#470 caress
Knocked on the door
What are you saying? Kipferon contains components of human blood, can you imagine how your body might react to this? Everything can just “play.” In a bad way. Do not risk!
Genferon is safe, it is made completely differently, there are no such components. You just need to apply it straight away and increase your immunity at the same time. (with them - candles, that is)
#471 light cat //
I saw the light in the window
#472 NotADoctor
I saw the light in the window
Chlamydia is not like herpes viruses, which cannot be treated, and when cured, they leave the body forever, and no IgG should be present! By the way, what they say that it still remains in the cells is not true, the cell dies due to the fact that chlamydia fed on this cell, and since there is a lot of it, all sorts of adhesions and “scars” are formed :)
Tetracyclines (doxycycline 100 mg * 2-3 times a day) days
Together with doxycycline, you can take metronidazole 250 (Trichopolum) 2-3 times a day, 1 tablet for a course of 10 days to relieve existing inflammation and pain in the lower abdomen.
Macrolides (azithromycin 500 (trade name Solutab) or jozomecin 500 (trade name Vilprofen)) days, 2-3 tablets per day (first dose 1g = 2 tablets).
There may be such a treatment regimen with vilprafen: 1 day - 2 grams (1st dose 1 gram = 2 tablets, 2nd dose - 1 tablet, 3rd dose - 1 tablet), 2-7 days - 1.5 g (1 tablet 3 times a day), 8-14 days -1g (2 times a day, 1 tablet)
*enzymes for better absorption of antibiotics, this is VobEnzyme, 5 tablets 3 times a day at least half an hour before meals, throughout the entire course of antibiotic therapy and 1 week after it, 3 tablets 3 times a day.
*Nystatin 3-4 tablets per day (some are prescribed expensive Orungal or fluconazole)
*milk thistle meal 1 teaspoon 5 times a day before meals or during meals. You can also drink burdock juice 50:50 mixed with honey, 2 tablespoons half an hour before meals in the morning on an empty stomach. This is to support the liver.
* local intravaginal suppositories Hexicon 1-2 suppositories per day (chlorhexedine to destroy intravaginal chlamydia).
*they also write that you need to pour 0.05% chlorhexedine solution 3 times a day into the urethra (with a syringe without a needle) 1-2 cubes (I don’t remember exactly), check this question yourself
*Lubricate the vulva area with hexicon gel 2-4 times a day.
All these measures are designed to prevent self-infection from occurring and a new cycle of chlamydia reproduction does not begin again.
Time zone: UTC + 3 hours
Strange chlamydia.
Registered: 25-01, 16:15
Registered: 12-01, 01:06
Registered: 25-01, 05:23
From: Novosibirsk
Chlamydia: catch and neutralize!
The head of the therapeutic department, Vladimir Markovsky, talks about the insidiousness of this pathogen.
– What are these conditions?
- Well, it’s clear what chlamydia’s entrance gate is: it’s sexually transmitted infection!
– But here you are wrong! Not only. The entry points for chlamydia are any mucous membrane (eyes, nose, pharynx, genitals). But predominantly it is still a sexually transmitted disease. This is chlamydial urethritis, which is very sluggish, often asymptomatic, especially in men. As a rule, the disease goes undetected. In women, chlamydia manifests itself more often; apparently, there is a more favorable environment for the proliferation of chlamydia.
The prescription of antibacterial drugs leads to the fact that the local process ends. It can also end spontaneously, due to the immune system. But in most cases, against the background of local improvement, the infection generalizes, that is, it leaves the site of the entrance gate and can persist somewhere for a very long time.
-Where is she hiding?
– In the blood, in the lymph nodes, in the joints. Recently, chlamydia has become a major surgical problem. It turns out that the so-called aseptic necrosis of the femoral head is directly related to chlamydial infection in almost half of the cases. This is not a classic inflammation, because chlamydia does not live in the bones, but it forms mucous cysts, and the bone seems to “foam.” This can lead to total destruction of the entire joint.
In general, there are many variants of chlamydial infection. Chronic chlamydial infection is a huge problem. One American researcher very aptly said that in human pathology there are only two types of diseases - infectious diseases and infectious diseases themselves.
– So those diseases that we have always considered non-infectious are actually caused by infection?
– These are conditions caused by chronic viral and bacterial infection. Even in the development of such a common disease as atherosclerosis, chlamydial infection plays an important role. The constant presence of the pathogen in the body causes immunodeficiency. After all, what is any chronic disease? This is a series of exacerbations and remissions. Another academician I.V. Davydovsky wrote that the remission phase is by no means a period of temporary health, because the cause, in this case chlamydia, has not disappeared anywhere. Therefore, the body, even in a state of remission, continues to fight it. This means that the immune system in atherosclerosis, and in other diseases, is always in the tension phase. Chronic infection is accompanied by the release of inflammatory regulators - cytokines, which are involved in the formation of atherosclerotic plaque. And chlamydia is often found in the plaques themselves.
– They say that the flu is terrible not in itself, but because of the development of complications. What's the deal with chlamydia?
– Chlamydia is dangerous precisely because of its consequences: it chronic diseases genitourinary tract, decreased erectile function, miscarriage, infertility. These are local complications. But there are also complications associated with damage to other organs. Here's an example: a young man, a junior sergeant of the railway troops, fell ill with acute chlamydial urethritis. As a result, he became blind in one eye and had to have a femoral head endoprosthesis installed, at the age of twenty! This is what chlamydia is. An incorrectly or incompletely treated infection poses a great danger to the body.
Since the infection tends to become chronic, there is always an immunodeficiency, an overstrain of the immune system, which will certainly affect it in the future: more early development atherosclerosis, bone destruction, formation of mucous cysts.
– It turns out that it’s correct that any of your diagnostic programs necessarily includes examining the patient for the presence of infections?
– This is one of the advantages of our clinic! Examination for the most pressing infections is necessary, because an infection, even if it does not cause it, always complicates the course of any disease. In terms of diagnosing chlamydia, this means analyzing a urogenital scraping using the PCR method and, of course, determining the titer of antibodies in the blood. Indeed, during a chronic process, the pathogen in the blood is in the L-form, so we rely here on antibodies. The titer is high - you need to treat!
– And how do you treat?
– Now the rule of treatment is a combination of antibiotics with rational immunotherapy. The sensitivity of chlamydia to antibiotics is known. The situation is worse with immunotherapy. Because the immune system is extremely complex, multifactorial, and there are no sufficient criteria to evaluate it; they are very expensive and, again, do not provide a complete picture of the state of immunity.
– Then the question arises, what is rational immunotherapy?
– This is a complex effect on the immune system. Treatment is prescribed depending on age, duration of the disease, presence of complications, etc. Prescriptions may include T-activin, polyoxidonium, interferon inducers, a vitamin complex, and others in various combinations. We increase the body's nonspecific resistance and actively use physiotherapy. Any patient can be helped here.
After all, the immune system recognizes everything, including L-forms of chlamydia, but its reserves are not always enough to fight chronic infection; for this it must be supported.
– After all that has been said, the guarantee of our health is probably complete abstinence?
- Not really! Total abstinence is not required, although moderation never hurts! The only guarantee of health is the state of immunity. After all, 10% of people have congenital immunodeficiency, they always get sick. 10% are people with strong immunity; they never get sick or get sick very rarely. And for 80% of people – including you and me – the immune system depends on conditions. This means that we need to create conditions under which the immune system would always guard our health. This is everything that strengthens the immune system, starting from the regimen, quitting smoking, etc., including the correct use of immunomodulators - rational immunotherapy.
So, despite all the insidiousness of the pathogen, we have something to answer: modern medicine can cope with chlamydia and its complications!
Levofloxacin for chlamydia reviews
Antibiotic resistance of Chlamydia trachomatis in vitro: methodological aspects and clinical implications
Is it true that Nolitsin should be taken for a month for prostatitis?
Between 1998 and 2005, levofloxacin use increased from 3.1 to 12.7 prescriptions per 1000 visits, and community-acquired uropathogenic E. coli resistance increased from 1% to 9%. It should be noted that strains resistant to levofloxacin were significantly more often resistant to other antibiotics compared to levofloxacin-sensitive strains (90% vs 43%).
Risk factors for the development of levofloxacin resistance in uropathogenic Escherichia coli strains included hospitalization and use of levofloxacin in the previous year.
Thus, in a number of US cities, particularly Denver, there has been a clear increase in the frequency of prescriptions of fluoroquinolones (and, in particular, levofloxacin) after changes in the policy of empirical treatment of UTIs, which led to a rapid increase in fluoroquinolone resistance in uropathogenic community-acquired strains of E. coli. The study authors note that before initiating empirical treatment for UTIs with fluoroquinolones, the risk factors of a particular patient should be carefully analyzed.
Johnson L., Sabel A., Burman W.J., Everhart R.M., Rome M., MacKenzie T.D., Rozwadowski J., Mehler P.S., Price C.S.
Emergence of fluoroquinolone resistance in outpatient urinary Escherichia coli isolates. Am J Med. 2008; 121(10):
(Throughout the years 74 medical centers 10 countries - Germany, Italy, France, Spain, Russia, Brazil, Poland, Hungary, Australia, Holland during the ARESC study isolated, identified and determined the sensitivity of uropathogens to 9 antimicrobial drugs in adult patients (n = 4264) aged with symptoms uncomplicated cystitis. In the Russian Federation, 8 centers from the European part of Russia took part in the study).
The ARESC study: an international survey on the antimicrobial resistance of pathogens involved in uncomplicated urinary tract infections.
Where does Floracid’s substance come from? Whose levofloxacin substances are registered in the Russian Federation? (we do not take into account the regulatory certificate received in June 2009 for the synthesis of the substance levo-CJSC Active Component, St. Petersburg; it is unlikely that the Obolenskaya pharmaceutical factory has purchased it yet)
Levofloxacin - instructions for use, analogues, price and reviews
Release form
1. Tablets 250 mg and 500 mg.
3. Solution for infusion 0.5%.
Levofloxacin – group
Levofloxacin – manufacturer
Levofloxacins from various manufacturers are often named by simply combining the name of the antibiotic with the manufacturer, for example, “Levofloxacin Teva”, “Levofloxacin-Stada”, “Levofloxacin-Tavanic”. Levofloxacin Teva is produced by the Israeli corporation Teva, Levofloxacin-Stada is produced by the Russian concern Nizhpharm, and Levofloxacin-Tavanic is a product of Aventis Pharma Deutschland GmbH.
Doses and composition
- sodium chlorine;
- disodium edetate dihydrate;
- deionized water.
Levofloxacin 250 mg and 500 mg tablets contain the following substances as auxiliary components:
- microcrystalline cellulose;
- hypromellose;
- primellose;
- calcium stearate;
- macrogol;
- titanium dioxide;
- iron oxide yellow.
Spectrum of action and therapeutic effects
Indications for use
Levofloxacin - instructions for use
Levofloxacin tablets (500 and 250)
- Sinusitis – take 500 mg (1 tablet) 1 time per day for 10 – 14 days.
- Exacerbation of chronic bronchitis - take 250 mg (1 tablet) or 500 mg (1 tablet) 1 time per day for 7 - 10 days.
- Pneumonia – take 500 mg (1 tablet) 2 times a day for 1 – 2 weeks.
- Infections of the skin and soft tissues (boils, abscesses, pyoderma, etc.) - take 500 mg (1 tablet) 2 times a day for 1 - 2 weeks.
- Complicated urinary tract infections (pyelonephritis, urethritis, cystitis, etc.) - take 500 mg (1 tablet) 2 times a day for 3 days.
- Uncomplicated urinary tract infections - take 250 mg (1 tablet) once a day for 7 - 10 days.
- Prostatitis - take 500 mg (1 tablet) once a day for 4 weeks.
- Intra-abdominal infection - take 500 mg (1 tablet) 1 time per day for 10-14 days.
- Sepsis - take 500 mg (1 tablet) 2 times a day for 10 - 14 days.
Solution for infusion Levofloxacin
1. saline solution.
2. 5% dextrose solution.
3. 2.5% Ringer's solution with dextrose.
4. solutions for parenteral nutrition.
- Acute sinusitis– administer 500 mg (1 bottle 100 ml) 1 time per day for 10 – 14 days.
- Exacerbation of chronic bronchitis– administer 500 mg (1 bottle 100 ml) 1 time per day for 7 – 10 days.
- Pneumonia
- Prostatitis– administer 500 mg (1 bottle of 100 ml) once a day for 2 weeks. Then they switch to taking 500 mg tablets once a day for another 2 weeks.
- Acute pyelonephritis– administer 500 mg (1 bottle 100 ml) 1 time per day for 3 – 10 days.
- Biliary tract infections– administer 500 mg (1 bottle of 100 ml) 1 time per day.
- Skin infections– administer 500 mg (1 bottle 100 ml) 2 times a day for 1 – 2 weeks.
- Anthrax – administer 500 mg (1 bottle of 100 ml) once a day. After stabilization of the person’s condition, transfer to taking Levofloxacin tablets. Take 500 mg tablets once a day for 8 weeks.
- Sepsis– administer 500 mg (1 bottle 100 ml) 1 – 2 times a day for 1 – 2 weeks.
- Abdominal infection– administer 500 mg (1 bottle 100 ml) 1 time per day for 1 – 2 weeks.
- Tuberculosis - administer 500 mg (1 bottle of 100 ml) 1 - 2 times a day for 3 months.
When a person’s condition is normalized, it is possible to intravenous administration solution of Levofloxacin, switch to taking tablets in the same dosage. Take antibiotic tablets for the remainder of the course of treatment.
Tablets and solution
1. CC is above 20 ml/min and below 50 ml/min – the first dosage is 250 or 500 mg, then take half of the initial dose, that is, 125 mg or 250 mg every 24 hours.
2. CC is above 10 ml/min and below 19 ml/min - the first dosage is 250 mg or 500 mg, then take half of the primary dose, that is, 125 mg or 250 mg once every 48 hours.
Overdose
Treatment of overdose must be carried out in accordance with the existing symptoms. It is necessary to eliminate pathological symptoms by using medications that act in this direction. Any dialysis options to accelerate the removal of Levofloxacin from the body are ineffective.
Interaction with other drugs
Levofloxacin eye drops
1. During the first two days, apply 1 to 2 drops into the eye every two hours, throughout the entire period of wakefulness. You can put drops in your eyes up to 8 times a day.
2. From the third to the fifth day, apply 1 – 2 drops 4 times a day to the eyes.
Levofloxacin for children
Use for the treatment of ureaplasma
Treatment of prostatitis
Levofloxacin and alcohol
Contraindications
- hypersensitivity, allergy or intolerance to the components of the drug, including levofloxacin or other quinolones;
- renal failure with CC less than 20 ml/min;
- epilepsy;
- the presence of tendon inflammation in the past during treatment with any drugs from the quinolone group;
- age under 18 years;
- pregnancy;
- breast-feeding.
Relative contraindications to the use of Levofloxacin in tablets and solution are severe renal dysfunction and glucose-6-phosphate dehydrogenase deficiency. in such cases, the drug should be taken under close medical supervision of the person’s condition.
Side effects
1. Often – observed in 1 – 10 people out of 100.
2. Sometimes - observed in less than 1 person out of 100.
3. Rare - observed in less than 1 person in 1000.
4. Very rare - observed in less than 1 person out of 1000.
The most common sexually transmitted disease is chlamydia. Treatment in women is complicated by the absence of severe symptoms in many cases. Meanwhile, the disease progresses and complications develop. Statistics show that over 140 million people are infected every year. What causes the disease, its symptoms, possible complications and what effective treatment exists for chlamydia in women will be discussed in this article.
What is chlamydia?
Chlamydia is a range of diseases caused by different types of the Chlamydia bacterium. These microorganisms cause skin diseases, pneumonia and other respiratory diseases. One type of chlamydia, namely Chlamydia trahomatis, contributes to the occurrence of urogenital chlamydia.
But usually at this stage, chlamydia is not treated in women; medications are not taken, since often the infected person is not aware of the disease due to the absence of symptoms. Meanwhile, the bacteria multiplies and new lesions appear. Incubation period Chlamydia infection lasts up to a month depending on the person’s immunity.
Routes of infection
Genital chlamydia is transmitted sexually. Oral contraceptives and interrupted sexual intercourse cannot protect against infection. Infection occurs in 70% of cases during unprotected intimate relationships with a partner who is a carrier of the bacteria.
Chlamydia is transmitted from an infected mother to a newborn child both in utero and during labor. In medical science, there is controversy over the possibility of household transmission of the bacterium through shared personal hygiene products and underwear. It is known that chlamydia can exist in the external environment for up to 2 days. They die only when treated with high temperature. But what is the probability of a person being infected in this case - there is no consensus.
Forms of the disease
In medicine, two forms of chlamydia are distinguished depending on the degree of damage and duration of the disease. Each of them has its own symptoms and individual treatment regimen. The classification is as follows:
- The fresh form affects the lower part of the genitourinary system. The duration of the disease is up to 2 months.
- When does bacteria spread to the lower urinary tract and how long does it last? life cycles over 2 months, then doctors diagnose " chronic chlamydia"Treatment in women in this case involves additional, often combined antibacterial drugs.
Medical statistics claim that in 67% of chlamydia infections, the disease is completely asymptomatic. In this case, the disease manifests itself only in the stage of chronicity and the development of complications with corresponding symptoms. Most often, pronounced symptoms appear only at an advanced chronic stage of chlamydia development and manifest themselves as follows:
- burning in urethra and vagina;
- itching of the genitals;
- cloudy discharge with an unpleasant odor;
- pain during urination;
- nagging pain in the lower abdomen;
- discomfort during sexual intercourse;
- spotting in the middle of the menstrual cycle;
- increased body temperature;
- menstrual irregularities.
Causes of chlamydia
The reasons for the large-scale spread of chlamydia are the lack of public awareness of the problem, especially among adolescents. Few people know how chlamydia is treated in women. The drugs needed to combat the disease, meanwhile, cause additional harm to the health of the young body, acting quite aggressively on it and having a number of side effects.
Contribute to infection with the bacterium: early onset of sexual activity, indiscriminate change of partners, sexual intercourse not protected by a condom.

Why is it dangerous for a woman?
This begs the question: what is so terrible about chlamydia, if in most cases the disease does not manifest itself with any pain symptoms? The answer is clear - the disease is dangerous due to its development serious complications. In the absence of the necessary treatment, chlamydia can affect the reproductive organs and contribute to the occurrence of the following pathological processes:
- cervicitis or inflammation of the cervix;
- pathological processes in the uterus, ovaries, fallopian tubes;
- adhesions in the pelvic organs;
- endometritis - endometrium of the uterus;
- cystitis and urethritis;
- as a consequence of complications - infertility.
The danger of chlamydia during pregnancy
Chlamydia is extremely dangerous in pregnant women. Treatment is complicated by the patient’s inability to take a number of necessary medications, since most of them can have an extremely negative impact on the development of the fetus. The asymptomatic course of the disease, and, accordingly, its late detection and untimely prescription of treatment can lead to complications or termination of pregnancy: fever, polyhydramnios, non-developing pregnancy, rupture of the membranes, miscarriage or premature birth. The likelihood of developing ectopic pregnancy if conception occurred in the presence of an infection in the woman’s body. In 30% of cases, the fetus is infected in utero, and in 40% the child is infected during passage through the birth canal.
How dangerous it is for a child

Diagnosis of chlamydia
A gynecologist may suspect the presence of an infection during a general examination using a speculum. He will be able to detect symptoms characteristic of most diseases of the reproductive system: inflammatory processes, areas of erosion, a large number of secretions, their corresponding consistency, color and smell.
To confirm the diagnosis and identify the causes of pathological processes, the specialist will take a smear from the vagina for bacteriological analysis. A general smear cannot detect the presence of chlamydia, but it will detect other sexually transmitted infections, which often develop in parallel with chlamydia.
A blood test to determine antibodies to chlamydia also cannot reliably confirm the diagnosis. Since the presence or absence of antibodies cannot reliably indicate the presence of living bacteria in the body.
PCR diagnostics are carried out to determine the DNA of chlamydia. The material for analysis is vaginal discharge. A positive test result will reliably confirm the presence of infection. But if negative, additional research is needed.
Bacterial culture is the most reliable way to detect chlamydia. The material for analysis (vaginal discharge) is placed in an environment favorable for chlamydia. Then, after the time necessary for the growth and reproduction of bacteria, the presence or absence of bacteria is determined under a microscope.

Treatment methods for chlamydia
The disease is treated with general and local methods. The main treatment for chlamydia in women is antibiotics. The treatment regimen is developed by the doctor on an individual basis. When choosing an antibacterial agent, the following factors must be taken into account:
In addition to antibacterial agents, immunomodulating drugs, probiotics, and enzymes are prescribed.

Treatment regimen for chlamydia
Once the diagnosis is confirmed, it is necessary to prescribe the correct treatment for chlamydia in women. The scheme is as follows:
1. Macrolides for the treatment of chlamydia are most effective:
- drug "Erythromycin": 0.5 g 4 times a day for 2 weeks;
- "Josamycin" product: 1 g once, then 0.5 g twice a day for 10 days;
- medicine "Spiramycin": three times a day, 3 million IU for 10 days;
- drug "Klacid": 250 mg twice a day for 14 days.
2. Fluoroquinolones are used less frequently, since many types of bacteria are resistant to this type of antibiotics:
- "Ofloxacin": one tablet twice a day for 10 days. If ineffective, the doctor may increase the dosage;
- medicine "Lomefloxacin": 1 tablet once a day, 10 days, used for uncomplicated forms of chlamydia;
- drug "Pefloxacin": 600 mg once for 7 days.
3. Broad-spectrum antibiotic “Clindamycin” is taken 2 tablets 4 times a day for a course of 7 days. This drug effectively treats chlamydia in women. Reviews indicate the majority of cases of complete cure and a minimal number of adverse reactions to the medicine.
Immunomodeling therapy helps the body strengthen its strength to fight infection when treating chlamydia in women. The drugs are prescribed as follows: Cycloferon in a course of 5 injections according to the prescribed regimen in parallel with taking antibiotics. And the drug "Neovir" of 7 injections of 250 ml every 48 hours after a course of antibiotics.
Antibiotics have an extremely negative effect on the microflora of the gastrointestinal tract. To prevent the development of stomach diseases, enzyme preparations and probiotics are prescribed: Bifidumbacterin, Lactobacterin, Chlorella, Hilak-Forte and others.

Local treatment of chlamydia
In addition to general therapy, the gynecologist prescribes local treatment chlamydia in women. Suppositories have anti-inflammatory and antibacterial properties. Dimexide solution is also used in the form of tampons, antibacterial gels and creams, and douching. To restore the body's strength, the doctor will prescribe a complex of multivitamins, for example "Supradin". While treating the infection, you must abstain from sexual intercourse or use a condom.
Physiotherapeutic procedures
In the treatment of chlamydia, especially in chronic form, effective additional treatment methods are physiotherapy methods:
- low frequency ultrasound;
- local laser phoresis;
- electrophoresis;
- UFOK.
Treatment of chronic chlamydia
If a doctor diagnoses chronic chlamydia, treatment in women involves the following regimen:
- Injections of the drugs "Neovir" or "Cycloferon" 7 times every other day.
- The drug "Rovamycin" is started to be taken at a dose of 3 million IU three times a day after the third injection of cycloferon. The course of treatment is 14 days.
- The drug "Diflucan" 1 capsule on the 7th and 14th day of treatment with the main antibiotic.
- Vitamin complexes.
- Physiotherapy procedures according to indications.
Treatment during pregnancy
- Antibiotic therapy as prescribed by a doctor: drugs "Erythromecin", "Rovamycin", "Sumamed".
- Immunomodeling therapy with the help of drugs, suppositories, which include substances such as myelopid, econazole nitrate or interferon.
- Probiotic preparations in the form of topical suppositories and oral agents.

Confirmation of cure
Since chlamydia rarely manifests itself with severe symptoms and one cannot judge by their absence effective treatment diseases, after completing a drug course to combat the infection, it is imperative to carry out control tests in several stages and using different methods:

Prevention of chlamydia
Chlamydia can cause serious complications. Treatment in women is carried out with antibacterial drugs that have an adverse effect on various internal organs. Preventive methods will help you avoid many health problems, namely: a responsible attitude towards your own health, which is manifested in the exclusion of promiscuous sex and the use of barrier methods of contraception and regular medical examinations. To prevent complications during pregnancy and during pregnancy planning, it is necessary to be tested for chlamydia and other sexually transmitted infections.
Chlamydia is insidious due to its asymptomatic nature and rapid spread. Therefore, the lack of treatment or independent attempts to fight the infection can lead to unforeseen consequences and serious impairment of the health of the infected person and his partner. Seeing a doctor will help prevent the development of complications and overcome the disease.
 How to recognize a witch - signs that warn of evil
How to recognize a witch - signs that warn of evil Dream interpretation dreamed of shit
Dream interpretation dreamed of shit How to squeeze a lemon: tips and methods How to squeeze juice from a lemon at home
How to squeeze a lemon: tips and methods How to squeeze juice from a lemon at home Employment agreement (contract) How to correctly draw up an employment contract with an employee
Employment agreement (contract) How to correctly draw up an employment contract with an employee DOA of the knee joints: stages, symptoms and treatment
DOA of the knee joints: stages, symptoms and treatment Dimexide - detailed description and use at home Dimexide if it enters the stomach
Dimexide - detailed description and use at home Dimexide if it enters the stomach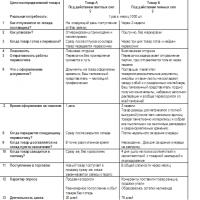 Andrey Stygar: How to make inventory profitable?
Andrey Stygar: How to make inventory profitable?