Trichomonas chronic in women symptoms. The main symptoms of chronic trichomoniasis in women. Treatment of the chronic form of the disease
Trichomoniasis (trichomoniasis) is the most common sexually transmitted disease. The causative agent of the infection is Trichomonas, which is a unicellular organism of the obligate type, that is, it is able to carry out its vital activity only in another organism. The microbial cell has a size of 15-30 microns, has formations in the form of mobile flagella. Trichomonas settles in the urethra in men.
Trichomoniasis, due to its specificity, is not always visually diagnosed in men. Very often there is a latent course of the disease. In some cases, there are very mild symptoms of irritation in the urethra and urethra, but they do not pay attention. There are cases when a false diagnosis was carried out, respectively, the treatment of the disease was not adequate. Such aspects lead to the chronic course of the disease.
Treatment of chronic trichomoniasis in men is carried out according to certain schemes and should include the treatment of concurrent infectious diseases of the genitourinary system.
This is due to the ability of the occurrence of mixed trichomonas infections.
The mechanism of infection with trichomoniasis and the features of the vital activity of Trichomonas
 Trichomoniasis of the urogenital type is transmitted sexually. The probability of infection through common hygiene products is minimal. Non-sexual transmission in rare cases is possible during childbirth, during a medical examination, when using a shared toilet seat in public toilets. Compared with the main mode of transmission of infection through sexual contact, other routes of infection occupy a small part of the total number of reported cases of the disease.
Trichomoniasis of the urogenital type is transmitted sexually. The probability of infection through common hygiene products is minimal. Non-sexual transmission in rare cases is possible during childbirth, during a medical examination, when using a shared toilet seat in public toilets. Compared with the main mode of transmission of infection through sexual contact, other routes of infection occupy a small part of the total number of reported cases of the disease.
Infection with trichomoniasis of a man through sexual contact with a sick woman occurs in 70-75% of cases. Due to the long incubation period of the disease, it can be 28 days, and also because of the latent course of the disease, extremely high opportunities for multiple spread of infection are created.
Trichomonas in men enters the mucous membrane of the genital organs, subsequently the pathogen grows and the urethra becomes completely infected. Lack of treatment leads to a chronic course of the disease. The secreted products of the activity of the microorganism lead to loosening of the internal tissues of the urethra, swelling and hyperemia occur, ulcerations are observed.
One of the main problems associated with the treatment of trichomoniasis is the problem of mixing infections. Trichomoniasis in the form of monoinfection is rare, in about 10% of all cases of the disease. The rest of the patients have mixed infections. Microorganisms that can be mixed with trichomoniasis:
- gonococci;
- chlamydia;
- fungal infections;
- ureaplasma;
- gardnerella.
As a result of the clinic and laboratory diagnostics, parallel infections are detected. It is important to clarify here that the treatment should be aimed at suppressing the growth of each individual type of pathogen in the body of a man.
Classic symptoms of trichomoniasis
The insidiousness of the disease is that if women show obvious signs of the disease in the form of abundant vaginal discharge, then in men most often this disease occurs without visible symptoms. Complaints about altered well-being are received as complications arise. This aspect should attract close attention, since preventive measures to identify Trichomonas make it possible to start treatment in a timely manner if necessary and prevent the transition of the disease to the chronic phase. This does not mean that every man is required to take certain tests and analyzes to detect trichomoniasis. In each individual case there is selectivity. That is, permanent partners in sexual life (husband and wife), who do not have trichomoniasis in the body, may not worry about the latency of the disease. If a man is sexually promiscuous, then the likelihood of infection increases significantly, and given the frequent absence of symptoms of the disease, prerequisites are created for periodic laboratory diagnosis.
 If the symptoms of the disease appear, then the man usually finds a slight burning sensation during urination, scanty discharge. Sometimes the symptoms of the disease resemble those of gonorrhea. Given the ability of trichomoniasis to mix infectious processes, any disease of the genitourinary system must be considered from the perspective of a mixed trichomonas infection.
If the symptoms of the disease appear, then the man usually finds a slight burning sensation during urination, scanty discharge. Sometimes the symptoms of the disease resemble those of gonorrhea. Given the ability of trichomoniasis to mix infectious processes, any disease of the genitourinary system must be considered from the perspective of a mixed trichomonas infection.
There is a theory about the possibility of self-healing of trichomoniasis. The basis of this theory is that trichomoniasis in men can last for about 4-5 weeks, then there is a self-healing from the infection only due to the immune system. To successfully complete this process, you need:
- reliable information about monoinfection (complete absence of other diseases of the genitourinary system);
- the impossibility of sexual relations for the entire designated period;
- the immune system of a sick person must be able to resist the disease;
- the pathogen should not have increased resistance to the protective functions of a particular organism.
The above points show the doubtfulness of this theory, since it is impossible to foresee these provisions in advance. Protracting the disease in the hope of self-healing usually leads to a chronic phase and complications.
The pathological infectious process is characterized by inflammatory symptoms of lesions of the urogenital tract:
- - inflammation of the urinary canal. The main symptom is light discharge of a mucous nature. Redness of the urethral lips is also noted.
- Prostatitis- Inflammation of the prostate gland with periodic pain, which may increase during sexual arousal.
- Cystitis- inflammation of the bladder mucosa, which is manifested by increased urination, burning, the appearance of mucus in the urine.
- Vesiculitis- inflammation of the seminal vesicles, which affects the quality of sperm.
- Orchitis- inflammation of the testicles, which clinically does not manifest itself in any way, but leads to a violation of spermatogenesis (maturation of spermatozoa) and male infertility. With a weakened immune system, the infection can spread upward and affect the kidneys with the development of pyelonephritis.

For men, the following symptoms are characteristic:
- Itching in the penis;
- Pain when urinating;
- The appearance of whitish or gray discharge from the urethra;
- The development of hyperemia of the genital organs;
- Blood streaks can be found in the ejaculate.
In men, the symptoms are vague, therefore, most often, they are found during examination of the priest for prostatitis or other problems.
Chronic trichomoniasis in women
- Pain
- Swelling and inflammation of the vagina;
- Pain during intercourse;
- Foamy, with an unpleasant odor, yellow-colored discharge;
- Intermenstrual spotting spotting,
- erosion development.
- Trichomonas are the main cause of the subsequent complicated course of pregnancy with its termination in the early stages.

Due to the fact that trichomoniasis has a primary chronic course with minimal or no symptoms, to identify the pathogen.
Chronic trichomoniasis: diagnosis
The presence of trichomoniasis cannot be determined only by the described symptoms.
For diagnosis, use laboratory diagnostics.
Methods for diagnosing the disease:
- smear microscopy;
- bacteriological research;
- PCR - diagnostics;
- Serology.
Let's deal with each method separately.
Allows you to identify the DNA of the pathogen from the taken biomaterial.
Microscopy- serve to identify the pathogen by applying to a glass slide and staining the material.
The resulting smear is then examined under a microscope.
Bacteriological culture.
It is carried out by placing a biomaterial on a nutrient medium.
Serological method- determination of the presence in the blood of antibodies to Trichomonas.
Note! Before going to the laboratory, you should take a referral for analysis from a specialist doctor.
In order to pass the tests correctly, you must:
- Men do not urinate before analysis for 2-3 hours;
- For women, the analysis is not carried out during menstruation;
- Before analysis, do not use candles and douching;
- Exclude sexual contacts.
Chronic trichomoniasis: complications
With untimely treatment, a number of serious complications may develop, both for women and men.
For men, complications of this disease are fraught with the development of serious lesions of the prostate gland.
Possible formation of cysts.
There will be problems in sexual life.
For women, an ectopic pregnancy is possible.
Inflammatory processes on the cervix, cysts and erosion.
Trichomoniasis chronic - treatment
To prevent re-infection, treatment should be carried out by two partners at the same time.
The main method of treating pathology is therapy, which is aimed at the destruction of causative agents of trichomoniasis.
For this, antitrichomonas drugs are used.
Since Trichomonas are protozoa, the use of antibiotics to destroy them is ineffective.
Chronic trichomoniasis in the treatment is necessarily included
In chronic trichomoniasis, treatment must include:
- I. Local treatment (baths, canal washing)
- II. Enzymes
- III. Immunomodulators
- IV. anti-inflammatory
Attention! Before treatment, you should first consult with your doctor.
After the course of treatment, laboratory monitoring of its effectiveness is mandatory.

If a diagnosis of chronic trichomoniasis in women is established, treatment should begin as early as possible.
Since in a subsequent pregnancy there is a high risk of its interruption.
Therefore, it is better to plan a pregnancy only after a laboratory examination has confirmed that the woman has cured chronic trichomoniasis.
With the development of chronic trichomoniasis in men and women, please contact the author of this article - a venereologist, urologist in Moscow with 15 years of experience.
Preventive measures for trichomoniasis
Preventive measures for trichomoniasis are similar to any other sexually transmitted diseases.
Prevention includes:
- Use of barrier contraceptives;
- In case of dangerous sexual intercourse, consult a doctor;
- During the treatment of the disease, to exclude infection of family members;
- Do not self-medicate.
If it was not possible to avoid infection with Trichomonas, you should immediately seek advice and diagnostic tests from a venereologist.
If we summarize all the knowledge about lichen that a simple layman has, it turns out that lichen is contagious and can be transmitted from contact with an infected carrier. This, of course, is true, but everything is somewhat more complicated and diverse.
Lichen is a general definition of a whole group of skin diseases. The name itself is used both in medical terminology and in ordinary language.
In the people, the term lichen is more used when talking about a skin ailment picked up from contact with an infected animal, and ringworm most often falls under this case. In the medical environment, lichen is not only a ringworm, it is the whole category of the disease, which has similar symptoms, these are: a change in the pigmentation of the damaged skin area, peeling and itching.
Lichen transmission can be divided into: infectious and contagious. Depending on the type of skin lesion, the disease itself proceeds, its treatment and the likelihood of relapse.
Identified causative agents of lichen are some microbes, as well as several varieties of microscopic fungi.
First of all, speaking of fungi, we mean the species of zooanthropophilic fungi. It is this fungus that can equally successfully survive both on the human body and on the animal. In fact, this fungus is the cause of the transmission from animals to humans of ringworm.
Anthropophilic type of fungus, this is the next variety that is transmitted from contact between people, or with the clothing of an infected person.
Lichen simple, treatment of white lichen
Given that white lichen disappears on its own, most people are not interested in treatments.
In connection with the violation of white deprive the aesthetic appearance of the skin, it is treated more like a cosmetic problem, respectively, skin softening ointments or a simple baby cream are used in the treatment.
In winter, from the cold, the skin dries up, and white lichen may appear more clearly. In this case, it is possible to use a hormonal ointment.
When using only the above cosmetics, white lichen can completely disappear. If this does not happen, it is worth contacting a dermatologist again for a detailed analysis and identification of the true origin of white spots.
And yet, white lichen is not contagious, it is not transmitted from the carrier to another person, and being a benign neoplasm, it is completely unaffected.
How to avoid getting sick
There are no exact rules for the prevention of white lichen, but we can still offer a number of recommendations:
- It is necessary, if possible, to avoid injuries to the skin, and in case of damage to the skin, treat the injury with antiseptic agents and apply a plaster;
- Do not use personal belongings of an infected person, combs, towels, washcloths;
- Monitor immunity. Try to keep it at a high enough level;
- Avoid stressful situations, especially of a prolonged nature;
- Include antiviral foods in the diet, and these are: garlic, onions, citrus group, carrots, beets;
- Taking decoctions of herbs.
And, of course, the main weapon of prevention is always a timely appeal to a dermatologist in the event of the first signs of white, lichen simplex.
READ ALSO
No related posts.
(trichomoniasis) is a sexually transmitted infection that causes inflammation of the organs of the genitourinary system. Manifested by signs of colpitis, urethritis, cystitis, proctitis. Often combined with other genital infections: chlamydia, gonorrhea, mycoplasma, candidiasis, etc. In the acute stage, abundant vaginal discharge, itching and burning in women and pain during urination in men are noted. In the absence of adequate treatment, it becomes chronic and can later cause prostatitis, infertility, complicated pregnancy and childbirth, childhood pathology and mortality.

General information
(or trichomoniasis) urogenital is a disease exclusively of the human genitourinary system. The causative agent of trichomoniasis is vaginal (vaginal) Trichomonas, sexually transmitted.
The target organs of trichomoniasis in men are the urethra, prostate, testicles and their appendages, seminal vesicles, and in women - the vagina, the vaginal part of the cervical canal, the urethra. Trichomonas vaginalis in women is found more often due to more pronounced manifestations of trichomoniasis and more frequent visits to the doctor for preventive purposes. Basically, trichomoniasis affects women of reproductive age from 16 to 35 years. During childbirth, infection with trichomoniasis of a newborn from a sick mother occurs in about 5% of cases. In newborns, trichomoniasis occurs in a mild form due to the structural features of the epithelium and is able to heal itself.
In men, usually, the presence of trichomonas does not cause obvious symptoms of trichomoniasis, they are often carriers of trichomonas and, without experiencing obvious discomfort, transmit the infection to their sexual partners. Trichomoniasis can be one of the causes of non-gonococcal urethritis, chronic prostatitis and epididymitis (inflammation of the epididymis), contribute to the development of male infertility due to a decrease in sperm motility and viability.
Infection with trichomoniasis mainly occurs through sexual contact. Household way - through contaminated linen, towels, swimwear, trichomoniasis is transmitted extremely rarely.
The number of diseases associated with trichomoniasis is large. Trichomoniasis is often detected with other STI pathogens (gonococci, chlamydia, ureaplasmas, Candida fungi, herpes viruses). It is now believed that Trichomonas contribute to the development of diabetes, mastopathy, allergies, and even cancer.

Biological features of the causative agent of trichomoniasis
Trichomonas are fixed in the cells of the mucous membrane of the urinary tract and cause an inflammatory process there. Trichomonas waste products poison the human body, reduce its immunity.
Trichomonas can live in the genitals and even in the bloodstream, where they penetrate through the lymphatic pathways, intercellular spaces with the help of the enzyme hyaluronidase. Trichomonas are extremely adapted to existence in the human body: they can change shape, disguise themselves as blood plasma cells (platelets, lymphocytes) - which makes it difficult to diagnose trichomoniasis; "cling" to other microbes and in this way evade the body's immune attack.
Microorganisms (gonococci, ureaplasmas, chlamydia, fungi of the genus Candida, herpes viruses, cytomegalovirus), getting inside Trichomonas, find protection there from the action of drugs and the human immune system. Mobile Trichomonas can spread other microbes through the genitourinary system and through the blood vessels. By damaging the epithelium, Trichomonas reduce its protective function, and facilitate the penetration of microbes and sexually transmitted viruses (including HIV).
Trichomonas carriage is isolated as a form of trichomoniasis, in which the pathogen is detected in the laboratory, but there are no manifestations of the disease. This division is conditional, since different forms of trichomoniasis can pass into each other. Erased forms of trichomoniasis play a large role in the spread of the disease. The pathogen living in the genitourinary system is a source of infection for a partner during intercourse and its own re-infection.
Trichomoniasis is dangerous for its complications, because it increases the risk of transmission of other infections (including HIV), pregnancy pathologies (premature birth, stillbirth), the development of infertility (male and female), cervical cancer, chronic diseases of the genitourinary system. In the presence of similar symptoms, and even in the absence of them, it is necessary to be examined for trichomoniasis, and possibly other STIs. This is important for women planning pregnancy, for sexual partners - Trichomonas carriers and patients with trichomoniasis; for everyone leading an active sex life.
Self-treatment of trichomoniasis can lead to the opposite result: Trichomonas become more aggressive, begin to multiply more actively, while the disease acquires hidden or atypical forms. Diagnosis and treatment of trichomoniasis in this case is much more difficult.
Diagnosis of trichomoniasis
Diagnosis of trichomoniasis is to detect the pathogen using various methods.
Based on the complaints of patients and examination, it is possible to suspect the presence of Trichomonas. When examining women with trichomoniasis, signs of inflammation are observed - swelling and hyperemia of the vulva and vagina. During colposcopy, a symptom of "strawberry cervix" can be observed: redness of the mucosa with pinpoint and focal hemorrhages on the cervix. Dysplasia of the epithelium is noted, sometimes the appearance of atypical epithelial cells is possible.
Reliably trichomoniasis is detected using laboratory methods:
- microscopy of the test material (for women - smears from the vagina and urethra, for men - smears from the urethra);
- cultural (microbiological) method using artificial nutrient media;
- immunological method;
- PCR - diagnostics.
Trichomoniasis in men is more difficult to diagnose, due to the lack of symptoms, in addition, trichomonas in this course of the disease are in an atypical amoeboid form. Before planning a pregnancy, both a man and a woman should undergo a complete examination for STIs, including trichomoniasis.
Treatment of trichomoniasis
Treatment of trichomoniasis is carried out by venereologists, gynecologists and urologists. It must be carried out in any form of the disease, regardless of the presence or absence of manifestations. Treatment of trichomoniasis should be carried out simultaneously for sexual partners (even with negative analyzes of one of them). Treatment of trichomoniasis in only one of the sexual partners is ineffective, since re-infection may occur after treatment. The production of antibodies against the causative agent of trichomoniasis does not form a stable immunity; after treatment, you can get sick again when re-infected.
Treatment of trichomoniasis must be combined with the treatment of other STIs that often accompany the disease.
Trichomoniasis is considered cured when the pathogen is not detected during diagnosis and no clinical symptoms are observed. Sexual life during treatment is excluded. It is necessary to inform your sexual partner about the presence of trichomoniasis and other STDs, about the need for examination and treatment.
The result of treatment of trichomoniasis depends on the normalization of the microflora of the genitourinary system and the body as a whole. In women, for this purpose, a vaccine against inactivated lactobacilli acidophilus is used. Perhaps the appointment of immunomodulatory drugs.
Andrey Viktorovich Zhuravlev
Candidate of Medical Sciences, doctor of the highest category

Trichomonas - the causative agent of trichomoniasis
Trichomoniasis is a sexually transmitted disease. The disease affects the genitals and urinary tract. The causative agent of the process is Trichomonada vaginalis.
Trichomoniasis most often occurs in an acute form with a vivid clinical picture.
But if the primary disease was treated incorrectly or not treated at all, the disease becomes chronic. This form of trichomoniasis is much more difficult to cure.
The reasons and general information are well described in our other articles:
Favorable conditions for the development of bacteria are the acidity of the environment of 5.9-6.5 pH and a temperature of about 36 degrees Celsius.

Reproduction of bacteria on the walls of the vagina
The acute form becomes chronic in 2-3 months from the moment of infection. This type of trichomoniasis is manifested by rare desuric disorders, pain in the lower abdomen and discomfort during sexual intercourse.
What leads to process chronization:
- decreased immunity;
- lack of timely treatment;
- therapy was inappropriate, or the patient did not drink all the necessary drugs to the end;
- the presence of other inflammatory diseases of the urogenital tract;
- promiscuity without protection.
In addition to the chronic form of the disease, trichomonas carriers are also possible. In this case, cultures for bacteria will be positive, but the patient does not show symptoms of trichomoniasis at all. This type of disease is need to be treated.
Diagnosis of the disease
Trichomoniasis is diagnosed by finding the bacteria in a vaginal or urethral swab.

Colonies of bacteria on a nutrient medium
Several diagnostic methods are possible:
- microscopy of an unstained preparation;
- inoculation of material on nutrient media;
- staining with methylene blue or Romanovsky-Giemsa followed by microscopy;
- PCR diagnostics.
Although microscopy gives a reliable result, the analysis should be carried out two or three times, since one of the results may be a false negative.
In men, it is much more difficult to find Trichomonas, because they often acquire an atypical form.
A dermatovenereologist, a urologist for men or a gynecologist for women is engaged in the treatment and diagnosis of the disease.
Treatment of the chronic form of the disease
Self-treatment for trichomoniasis is unacceptable: this can lead to the development of an aggressive form of the disease. Bacteria will take on an atypical appearance, and it will be much more difficult to deal with them.
Therapy of the infection is necessarily carried out in both sexual partners (even if the smears of one of them are negative). Sexual contacts are prohibited not only until the end of treatment, but the entire control period (to avoid reinfection - re-infection).
Treatment of chronic trichomoniasis consists of local and general therapy.
General therapy
Analogues of Metronidazole - Trichopolum, Rosex, Ornidazole.
Reception regimens for the chronic form, options:
- 500 mg 2 times a day for 7-10 days;
- the first day - 750 mg 4 times a day, the second - 500 mg twice a day. Only 5 g of Metronidazole in 2 days;
- 500 mg solution intravenously drip 3 times a day for 5-7 days.
The following drugs have a similar effect:
All of these drugs are strong enough, because they have side effects: nausea, vomiting, dizziness, heartburn, weakness, drowsiness. In addition, they absolutely incompatible with alcohol.
 Most likely, one course for chronic trichomoniasis will not be enough. On the recommendation of the doctor, the medication can be repeated.
Most likely, one course for chronic trichomoniasis will not be enough. On the recommendation of the doctor, the medication can be repeated.
Additionally, the doctor prescribes immunomodulating agents: Viferon, Immunal, Grippferon. Duration of admission - 7-10 days.
Local therapy
Women with trichomonas vulvitis or vaginitis can be placed in the vagina, Terzhinan: 1 vaginal tablet at night for 10 days.
The urethra can be washed with a 0.5% solution of silver nitrate or a 2% solution of protargol. The procedure is carried out every other day for 2 weeks. Before washing, you need to take a shower, it is better to spend it at night.
Douching (washing) of the vagina with herbal antiseptics (infusions of chamomile, sage, thuja cones, birch buds, calendula) gives a positive effect. The duration of treatment is 7-9 days. Then you need to take a break.
Lifestyle during therapy
At the time of treatment, the patient is advised to follow a diet: give up spicy, salty, spicy foods and alcohol. You can also limit sweets, chocolate, coffee and strong tea.
It is very important to observe personal hygiene. Shower twice a day, change underwear every day. Bed linen and towels should be individual for each family member to avoid spreading the infection.
Trichomoniasis is considered cured if, within 2 months after the therapy, smears for Trichomonas give a negative result.
Disease prevention
To avoid the formation of chronic trichomoniasis, you need to treat an acute infection in time. Therefore, if you have any pathological symptoms associated with the urogenital tract, you should consult a doctor for diagnosis.
Prevention of any sexually transmitted infections is as follows:

- avoid casual sexual contact;
- always use condoms;
- observe personal hygiene;
- underwear and towels must be for individual use.
See a doctor in a timely manner to identify any diseases at an early stage and begin treatment.
 Does ureaplasma pass by itself (can it pass on its own)?
Does ureaplasma pass by itself (can it pass on its own)? PCR analysis to detect chlamydia Chlamydia PCR how to do
PCR analysis to detect chlamydia Chlamydia PCR how to do COCs with different daily dosages: how to choose, an overview of the best drugs
COCs with different daily dosages: how to choose, an overview of the best drugs Ureaplasma parvum: characteristics, tests, symptoms in women and men, what is dangerous, whether it is necessary to treat
Ureaplasma parvum: characteristics, tests, symptoms in women and men, what is dangerous, whether it is necessary to treat Basic technologies for obtaining nanomaterials
Basic technologies for obtaining nanomaterials How to tell the time in English?
How to tell the time in English?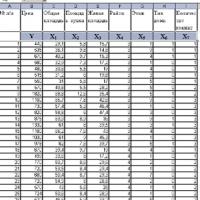 Introduction to Multivariate Statistical Analysis
Introduction to Multivariate Statistical Analysis