Whether there can be spotting at a spiral. Intrauterine devices - answer questions and debunk myths. Complications and side effects of IUD insertion
Prevention of unwanted pregnancy, or contraception, helps a woman maintain her health:
- reduces the frequency of abortions;
- helps to plan pregnancy and prepare for it;
- in many cases, it has an additional therapeutic effect.
One type of contraception is intrauterine. It is used most often in China, the Russian Federation and Scandinavia. In everyday speech, the concept of "intrauterine device" is often used.
Advantages of intrauterine contraception:
- relatively low cost;
- long period of use;
- rapid restoration of the ability to bear children after the removal of the spiral;
- the possibility of use during breastfeeding and with concomitant diseases;
- therapeutic effect on the endometrium (when using a hormonal intrauterine system);
- preservation of the physiology of sexual intercourse, lack of preparation, fullness of sensations during intimacy.
Types of intrauterine devices
Means for intrauterine contraception are of two types:
- inert;
- medical.
Inert intrauterine contraceptives (IUDs) are plastic products of various shapes that are inserted into the uterine cavity. Their use has not been recommended since 1989, when the World Health Organization declared them ineffective and dangerous to women's health.
Currently, only coils containing metals (copper, silver) or hormones are used. They have a plastic base of different shapes, close to the shape of the inner space of the uterus. The addition of metals or hormonal agents can increase the effectiveness of the coils and reduce the number of side effects.
In Russia, the following VMCs have gained the greatest popularity:
- Multiload Cu 375 - has the shape of the letter F, covered with a copper winding with an area of 375 mm 2, designed for 5 years;
- Nova-T - in the form of the letter T, has a copper winding with an area of 200 mm 2, designed for 5 years;
- Cooper T 380 A - copper-containing T-shaped, lasts up to 8 years;
- hormonal intrauterine system "Mirena" - contains levonorgestrel, which is gradually released into the uterine cavity, providing a therapeutic effect; calculated for 5 years.
Less common are IUDs that secrete medroxyprogesterone or norethisterone.


Which intrauterine device is better?
This question can be answered only after an individual consultation, taking into account the woman's age, her state of health, smoking, the presence of gynecological diseases, future pregnancy planning and other factors.
Mechanism of action
The principle of operation of the intrauterine device is the destruction of spermatozoa and the violation of the process of attachment of the embryo in the uterine cavity. Copper, which is part of many IUDs, has a spermatotoxic effect, that is, it kills spermatozoa that have entered the uterus. In addition, it enhances the capture and processing of spermatozoa by special cells - macrophages.
If fertilization does occur, the abortive effect of the contraceptive begins, preventing the implantation of a fertilized egg:
- contractions of the fallopian tube increase, while the fertilized egg enters the uterus too quickly and dies;
- the presence of a foreign body in the uterine cavity leads to aseptic (non-infectious) inflammation and metabolic disorders;
- as a result of the production of prostaglandins in response to a foreign body, the contractility of the walls of the uterus is activated;
- when using an intrauterine hormonal system, endometrial atrophy occurs.
The Mirena intrauterine system constantly secretes the hormone levonorgestrel at a dose of 20 mcg per day from a special reservoir. This substance has a progestogenic effect, inhibits the regular proliferation of endometrial cells and causes its atrophy. As a result, menstruation becomes scarce or completely disappears. Ovulation is not disturbed, the hormonal background does not change.
Is it possible to get pregnant if there is an intrauterine device? The effectiveness of intrauterine contraception reaches 98%. When using copper-containing products, pregnancy occurs in 1-2 women out of a hundred within a year. The effectiveness of the Mirena system is several times higher, pregnancy occurs in only 2-5 women out of a thousand during the year.

How to put an intrauterine device
Before inserting an IUD, you need to make sure that you are not pregnant. The procedure can be carried out regardless of the phase of the menstrual cycle, but best of all on the 4th-8th day of the cycle (counting from the first day of menstruation). Be sure to analyze smears for microflora and purity, as well as ultrasound to determine the size of the uterus.
The procedure takes place on an outpatient basis without anesthesia. This is a virtually painless procedure. In the first days after the introduction of the spiral, aching pains in the lower abdomen caused by uterine contractions may disturb. The first and 2-3 subsequent periods may be heavy. At this time, spontaneous expulsion of the spiral is not ruled out.
After artificial abortion, the spiral is usually installed immediately after manipulation, after childbirth - after 2-3 months.
The introduction of an IUD after a caesarean section is carried out six months later to reduce the risk of infectious complications. Spirals can be used during breastfeeding, which is their great advantage.
After the introduction of the IUD for a week, a woman is prohibited from:
- intense physical activity;
- hot baths;
- taking laxatives;
- sex life.
The next examination is scheduled for 7-10 days, and then in the absence of complications after 3 months. A woman should independently check the presence of IUD threads in the vagina after each menstruation. An examination by a gynecologist is enough to pass once every six months, if there are no complaints.
Removal of the intrauterine device
Removal of the IUD is carried out at will, with the development of certain complications or after the expiration of the period of use. In the latter case, you can introduce a new contraceptive immediately after removing the previous one. To remove the IUD, an ultrasound is first performed and the location of the helix is clarified. Then, under the control of a hysteroscope, the cervical canal is expanded and the spiral is removed by pulling on the "antennae". If the "antennae" breaks off, the procedure is repeated in the hospital. If the intrauterine device penetrates the uterine wall and does not cause complaints, it is not recommended to remove it unnecessarily, as this can lead to complications.
Complications of intrauterine contraception
Side effects of the intrauterine device:
- pain in the lower abdomen;
- genital infection;
- uterine bleeding.
These symptoms do not develop in all patients and are considered complications.
Pain in the lower abdomen
Occur in 5-9% of patients. Cramping pain, accompanied by bloody discharge, is a sign of spontaneous expulsion of the IUD from the uterine cavity. To prevent this complication in the period after the introduction, nonsteroidal anti-inflammatory drugs are prescribed.
Constant intense pain occurs if the contraceptive does not match the size of the uterus. In this case, it is replaced.
Sudden sharp pains may be a sign of perforation of the uterus with the penetration of part of the spiral into the abdominal cavity. The frequency of this complication is 0.5%. Incomplete perforation often goes unnoticed and is diagnosed after unsuccessful attempts to remove the IUD. With complete perforation, an emergency laparoscopy or laparotomy is performed.
genital infection
The frequency of infectious and inflammatory complications (and others) ranges from 0.5 to 4%. They are difficult to tolerate, accompanied by severe pain in the lower abdomen, fever, purulent discharge from the genital tract. Such processes are complicated by the destruction of the tissues of the uterus and appendages. For their prevention, broad-spectrum antibiotics are prescribed for several days after the introduction of the IUD.
Uterine bleeding
uterine bleeding develops in 24% of cases. Most often it is manifested by heavy menstruation (menorrhagia), less often - intermenstrual blood loss (metrorrhagia). Bleeding leads to the development of chronic iron deficiency anemia, manifested by pallor, weakness, shortness of breath, brittle hair and nails, and dystrophic changes in internal organs. To prevent bleeding, two months before the installation of the spiral and within 2 months after that, it is recommended to take combined oral contraceptives. If menorrhagia results in anemia, the IUD is removed.
The onset of pregnancy
IUD reduces the likelihood of pregnancy. However, if it does occur, the risk is higher than among other women.
If pregnancy occurs during the period of using the spiral, there are three scenarios for the development of events:
- Artificial termination, because such a pregnancy increases the risk of infection of the embryo and in half of the cases ends in spontaneous abortion.
- Removal of the IUD, which can lead to spontaneous abortion.
- Preservation of pregnancy, while the spiral does not harm the baby and is released along with the fetal membranes during childbirth. This increases the risk of pregnancy complications.
The ability to conceive and bear a child is restored immediately after the removal of intrauterine contraception, pregnancy occurs within a year in 90% of women who have not used other methods of contraception.
Indications for use
This type of contraception in nulliparous women can cause serious complications that prevent future pregnancy. An intrauterine device for nulliparous women can be used only if it is impossible or unwilling to use other methods. For such patients, mini-coils containing copper are intended, for example, Flower Cuprum.
It does not make sense to install an IUD for a short time, so a woman should not plan a pregnancy for the next year or longer.
IUDs do not protect against sexually transmitted diseases. On the contrary, they are believed to increase the risk of developing and worsen the course of such diseases.
Most often IUDs are used in the following situations:
- increased fertility, frequent pregnancies against the background of an active sexual life;
- temporary or permanent unwillingness to have children;
- extragenital diseases in which pregnancy is contraindicated;
- the presence of severe genetic diseases in a woman or her partner.
Contraindications to the intrauterine device
Absolute contraindications:
- pregnancy;
- endometritis, adnexitis, colpitis and other inflammatory diseases of the pelvic organs, especially acute or chronic with constant exacerbations;
- cancer of the cervix or body of the uterus;
- previous ectopic pregnancy.
Relative contraindications:
- uterine bleeding, including heavy menstruation;
- endometrial hyperplasia;
- congenital or acquired deformity of the uterus;
- blood diseases;
- severe inflammatory diseases of internal organs;
- previously occurring spontaneous expulsion (expulsion) of the IUD;
- intolerance to the components of the spiral (copper, levonorgestrel);
- no childbirth.
In these situations, the appointment of an intrauterine hormonal system is often justified. Its use is indicated for endometrial pathology, heavy bleeding, painful menstruation. Therefore, the gynecologist will be able to choose the right intrauterine device after examining and examining the patient.
There is a wide variety of contraceptives. Each has its positive and negative features. The introduction of an IUD - an intrauterine device - is very popular.
If this device was installed correctly, all the rules for its use are observed, then the use of the product is safe, does not cause discomfort and is 99% effective. But some girls, after installing the spiral, notice discharge mixed with blood. Their appearance may be physiological or pathological in nature, so you need to know about the symptoms of possible complications.
IUD Mirena is considered a highly effective means of protection against unwanted pregnancy. The active ingredient is levonorgestrel, a hormone that is released from the coil from the first day of establishment during the period of use. 20 mcg of the substance is released per day. After 5 years of use, the amount of hormonal content per day is 10 mcg.
Taking into account the physiological norms and characteristics of the female body, manufacturers have created a spiral from a core full of hormonal contents, a membrane responsible for its gradual release.
Before installing the device, one important rule must be taken into account: the items in the package are sterile, therefore, if its integrity is violated, it is necessary to refuse to use such a contraceptive. Otherwise, after the installation of the spiral, discharge may appear due to the addition of an infection, the spread of the inflammatory process.
It is also worth considering that due to the introduction of a hormonal drug, the body needs at least 3 months to get used to its action. The adaptation period may be accompanied by the appearance of spotting.
Types of spirals
Any intrauterine devices are made of polymers that are safe for the human body. For the purpose of contraception, a wide variety of products are used, which differ from each other in their shape, size characteristics, and principle of operation. T-shaped tools are considered the most popular, as they are very easy to use and install. At the free end of the Mirena body there is an annular loop, which is necessary for fixing the thread with which the IUD is removed.
Spirals are distinguished by the principle of action:
- neutral;
- medical;
- hormonal.
The neutral effect is that the introduced object is a foreign body that prevents embryonic development. Such funds are large, do not provide maximum effectiveness of protection against unwanted pregnancy. They also provoke, accompanied by severe pain. When these spirals are installed, very often women have uterine bleeding.

Medical IUDs are also divided into several groups depending on the material that was used in the manufacture of the contraceptive. Spirals may contain:
- copper;
- silver;
- gold.
Those products that contain copper are easy to install, they rarely cause any complications, including bleeding. But they have several contraindications, in which you should stop using:
- the presence of inflammation;
- diseases of the pelvic organs;
- cervical erosion.
It is worth noting that it is during the installation of the spiral that one should not underestimate, since this disease requires mandatory monitoring and treatment.
If a woman has a spiral, while there are scant brown discharges for a long time, it is necessary to consult a doctor in order to diagnose the development of complications against the background of undetected contraindications to the installation of the remedy.
Spirals with silver are distinguished by their antiseptic qualities, they fight the inflammatory process, and IUDs, which contain gold, are characterized by the fact that they do not corrode, they are fully combined with uterine tissues. Such products do not provoke the appearance of allergic reactions, complications. Gold-containing contraceptives are installed for a longer period.
The hormonal principle of the spirals is that they contain a hormone that is gradually sent to the uterus in order to provide a contraceptive effect. Such contraceptives are safe and do not cause side effects.
Spiral installation features
The Mirena coil is a hormonal system that is easy to install and has a low risk of complications. The principle of action is that it does not allow spermatozoa to penetrate into the upper areas of the female reproductive system, blocks the process of fertilization of the egg.

Also, after the installation of Mirena, cervical mucus thickens, which contributes to blockage. This principle of action allows you to maintain high efficiency of the product for a long time.
The installation procedure is quite fast, the woman does not experience any discomfort. If there are no contraindications, the gynecologist appoints the day of the procedure. Basically, the product is installed at the end of menstruation. It takes about 15 minutes. Fixing the IUD in the uterine cavity is painless, as local anesthesia is administered.
However, if bloody discharge has started from the uterus, and they last long enough, you should consult a doctor. This will prevent the development of complications.
They can be scarce, or vice versa, plentiful, so we advise you to read a separate article on this topic.
Complications and contraindications
Installation of the Mirena coil can be done even in adolescence. But before going for the procedure, it is necessary to exclude the possibility of contraindications:
- neoplasms in the female reproductive system;
- inflammation in the genitourinary system;
- uterine injury;
- bleeding with an unclear etymology;
- cardiovascular pathologies;
- diabetes.
In the absence of these contraindications, the risk of any complications is minimal, but it still remains if mistakes were made during the procedure.
There are several possible complications that may occur during and after the installation of the structure. Sometimes the introduction of the IUD provokes the penetration of pathogenic microorganisms into the body, the development of the inflammatory process. Because of this, it is often possible to observe the appearance of spotting, which has a greenish or yellowish tint and an unpleasant odor.
Also, a daub may appear when the established structure is rejected. Most often, such complications occur against the background of an incorrect arrangement of the helix.
Injury or puncture of the uterus causes bleeding. This happens extremely rarely. For the same reason, discharge may appear after removal of the IUD.
Pathological discharge
Regardless of the reason that provoked the appearance of a brown secret after the installation of Mirena, it is necessary to consult a doctor in order to eliminate the risk of developing possible complications. Such discharges are considered normal only when they do not have any foreign hue, unpleasant odor, are not accompanied by pain in the lower abdomen, lower back.
Such discharge in the first months after the installation of Mirena is caused by a violation of the uterine endometrium. If a woman regularly has mucus mixed with blood, and there is also other discomfort, she should urgently visit a doctor in order to diagnose pathological causes.
Bleeding
Abundant bleeding after the installation of Mirena is a sign of open uterine bleeding. Such a symptom may appear when the introduced contraceptive is rejected. In this case, the blood discharge will not have any specific odor, acquire a different color, for example, greenish or yellowish.

If severe bleeding occurs, you should immediately consult a doctor to diagnose the cause of this condition. But there is also a variant of the norm, when the discharge is physiological in nature. This applies to situations where brownish periods become more abundant. This state of the female body is a reaction to a hormonal drug, and gradually the menstrual cycle is getting better.
Injuries
Also, bleeding can be caused by trauma to the uterus, damage to the integrity of the vaginal mucosa.
You can recognize uterine bleeding by the abundance of discharge, the presence of pain in the lower abdomen. Sometimes it is so strong that it can only be stopped at a gynecologist's appointment or with the help of oral hemostatic drugs.
Damage to the genitals during the introduction of Mirena is rare and only through the fault of an unqualified doctor. Therefore, if abundant brown discharge appears during the installation of the spiral, it is urgent to consult a doctor.
Diseases of the reproductive system
Whitish or yellowish discharge, accompanied by an unpleasant odor, after installing Mirena can indicate diseases of the reproductive system. It is worth considering that the spiral itself does not entail their development, this condition can be caused by weakened immunity, stress, sexual intercourse with an infected partner.
Infection
After incorrect installation of the spiral, an infectious disease may develop. This happens if the doctor did not observe sterility, the woman neglected the rules of personal hygiene after the procedure.
The presence of infection of the genital organs is accompanied by the appearance of abundant secretions of a different nature, depending on the stage of development of the disease. They can be whitish, yellowish, bloody, greenish. They also have an unpleasant odor. In most cases, with an infectious lesion of the genital organs, the symptoms become pronounced before menstruation, and after menstruation they decrease.

If inflammation occurs after the installation of the spiral, brown discharge may appear. If they do not go away on their own after 2 days, you should immediately consult a doctor and start anti-inflammatory therapy.
Fixture offset
Brown discharge may appear when the Mirena is displaced. A change in the position of the spiral can be recognized by the presence of the following symptoms:
- cramping pains in the lower abdomen began;
- spotting is observed outside of menstruation, during sexual intercourse;
- there was a feeling of a spiral in the vagina.
It is worth considering that when displaced, Mirena does not provide maximum efficiency, while it can injure the cervix.
Ectopic pregnancy
When an IUD is inserted, there is a risk of an ectopic pregnancy. You can recognize such an abnormal location of the embryo by pain in the lower abdomen, the disappearance of menstruation or a change in their nature. In the case of such a pathology, there are discharges characterized by scarcity and short duration.
If you suspect an ectopic pregnancy, you should immediately consult a doctor. This is due to the fact that such a condition threatens the health of a woman.
Means for treatment
Treatment of the discharge that appears after the installation of the spiral will depend only on the cause of their occurrence. At the same time, only a doctor should diagnose pathologies and complications that have arisen, and he also prescribes the appropriate therapy.
If the discharge is caused by damage or rupture of the uterus, the contraceptive is removed, and the woman is prescribed anti-inflammatory, healing drugs or surgery. The method of treatment is prescribed taking into account the severity of the patient's condition.
If the discharge is a consequence of an infectious, bacterial or yeast infection of the genital organs, drug therapy is prescribed. The sooner the pathology is detected, the easier it is to cure.
If a woman fears the occurrence of the above complications, she should use other methods of contraception. You can give preference to oral contraceptive pills, condoms. Such funds do not provoke the appearance of secretions. In the first 3 months of taking OK, brown daub is allowed.
Many women are looking for reliable methods of contraception. To date, there are many pharmaceuticals, as well as gynecological products that help to avoid unwanted pregnancies. Intrauterine devices are considered a very popular method of contraception.
Unlike temporary contraceptives, intrauterine devices have a lasting effect. They can be set for a different period of time - from five to ten years. The principle of their action is very simple: they do not allow a mature egg to come out for fertilization. Spirals are of two types - hormonal and copper. Their cost is also different. It depends on the manufacturer, on the clinic where the spiral is placed.
The IUD (intrauterine contraceptive device) of the latest generation contains the hormone levonorgestrel. Every day, the daily rate of this hormone is released into the uterine cavity, which prevents pregnancy. Sometimes such spirals are introduced in the treatment of various gynecological diseases.
A bit of history
The Navy appeared relatively recently - only 80 years ago. Since then, they have become much better and more efficient. The first spirals had the form of a ring, plate or rod, which was made of precious metal. In the early 70s, doctors developed plastic flexible coils that protected against pregnancy, but had a lot of side effects. Women with such spirals often experienced heavy bleeding, pain and other phenomena.
With each subsequent decade, the design of spirals has improved. They became smaller and healthier. Today they are considered one of the best methods of contraception.
How the Navy works
It has already been said above that today there are two types of IUDs: hormonal and copper. Let's look at each of these types below:
Copper IUDs are made from a specific metal alloy. They inhibit the activity of spermatozoa. The uterus produces a fluid that destroys sperm and interferes with the fertilization of the egg. Such a spiral thins the walls of the endometrium. Such a spiral is put on for 10 years.
Hormone IUDs are very effective. Every day, a daily dose of a hormone is released from such a spiral, which provokes the release of mucus from the uterus and prevents the full attachment of the egg. Such spirals help in the treatment of certain gynecological diseases. They are set for 5 years.
What spirals look like and what are their advantages
Outwardly, both types of spirals are almost the same. They are made in the shape of the letter "T". At the heart of the spiral contains a container with a hormone. Metal spirals consist of a base on which copper or silver wire is wound.
Advantages of the IUD:
if the spiral is installed correctly, then it protects against unwanted pregnancy by 99%;
the spiral is inserted very quickly and easily - in just five minutes;
the spiral is placed for 5-10 years, which is very convenient for a woman;
spirals are affordable;
after a spiral, weight is not added, as after taking hormonal pills;
IUDs can be installed in those women who cannot take oral contraceptives;
the spiral begins to act as soon as it is installed;
after removing the spiral, the reproductive function will be restored and the girl will be able to become pregnant immediately.
Many girls think about what is better - oral contraceptives or a spiral? The spiral definitely wins. After all, with her you don’t have to worry about the fact that you took the pill at the wrong time. In addition, the spirals do not affect the figure in any way, which cannot be said about hormonal pills.
How is an intrauterine device inserted?
Before deciding on such a procedure, you need to find an experienced doctor. After all, efficiency will depend on this. It is best to choose doctors who have positive reviews about their work. Before sending the patient for such a procedure, the doctor will definitely conduct an examination. In some cases, it is necessary to take tests to make sure that there are no inflammatory processes.
A couple of days before the procedure, you must refrain from any sexual intercourse. In addition, douching, suppositories or pills should not be used unless prescribed by the doctor himself. It is best to insert an intrauterine device on the 1-7th day of menstruation, when the cervix is softer. Thanks to this, the spiral is introduced much easier.
The intrauterine device is installed in a sterile office on an outpatient basis. Installation time is only 5 minutes. Before the introduction of the spiral, the doctor treats the cervix with an antiseptic. During the introduction of the spiral, the girl may feel unpleasant tingling, pain in the abdomen. This is due to the fact that the doctor tightens the cervix with a special tool to straighten it. Such manipulations allow you to set the spiral in the correct position.
Immediately after administration, the woman may experience dizziness. Sometimes there is a sharp short-term pain. But these symptoms disappear on their own after half an hour after the installation of the spiral. If the symptoms do not disappear, the doctor re-examines the patient. It is possible that the helix was entered incorrectly. In such cases, it is removed and a new one is installed.
During the day after installation, the girl may feel aching pain in the lower abdomen. This is considered normal. Menstruation can also last - for two days. After the introduction of the spiral, in no case should you have sex for a week and you should not use tampons or any drugs, including aspirin.
After the introduction of the IUD, you can not go to the sauna, pool, beach or sunbathe in the sun (in the solarium). It is also worth giving up physical activity for a while. A month after the installation, you need to visit a doctor and do an ultrasound to see if everything is fine. If the spiral is placed correctly and the woman does not experience any discomfort, then she will simply need to visit the gynecologist twice a year in the future.
It's important to know
IUD can be installed after an abortion in the first menstruation.
If a woman had a miscarriage, then the spiral can be installed no earlier than a month and a half after that.
After childbirth, gynecologists do not recommend installing a spiral for the first three months. The body must recover.
The spiral must be removed in time - after five to ten years.
After removing the old spiral, you can immediately install a new one.
Every time after the end of menstruation, it is necessary to check the antennae of the spiral in the vagina. If the antennae are shorter or absent, then you should immediately contact a gynecologist.
For whom IUDs are contraindicated
An IUD can only be installed in women who have given birth. Also, this method of contraception is only suitable for those who have sex with one partner. After all, such a spiral can protect against pregnancy, but it does not protect against diseases that are sexually transmitted.
The spiral is not placed if the woman has inflammatory processes or gynecological diseases. Before installing the spiral, the patient must be examined. In no case should the spiral be installed during pregnancy, with malignant and benign tumors, with chronic diseases, with hormonal disorders, as well as with mastopathy.
Side effects
In the first time after the installation of the IUD, the following side effects may occur:
-
spiral loss;
inflammation of the mucous membrane of the cervix;
puffiness;
profuse menstruation;
backache;
increase in appetite;
absence of menstruation.
The intrauterine device is the most popular and effective female method of preventing unwanted pregnancy. In order to prevent complications, it is necessary to go through all the examinations and contact only a professional doctor; self-introduction of the spiral is not allowed. But even compliance with all conditions does not guarantee absolute smoothness. It happens that after the installation of the spiral, blood flows, this happens for various reasons. Everything about the procedure for introducing a spiral and complications in this article.
An intrauterine device is a special device consisting of an inert plastic and some metal (copper or silver), small in size. This device is inserted into the uterine cavity and prevents the girl from becoming pregnant. When, fertilization with an IUD can occur, but the spiral will not allow the embryo to attach to the endometrium of the uterus, the principle of action is similar to an abortifacient. A spiral is introduced to a girl on the 3rd or 4th day of menstruation, while the cervix is open.
Kinds
Today, 2 types of intrauterine device are actively used:
- Copper Navy. A copper coil inserted into the uterus releases copper ions, acidifying the environment of the uterus and reducing sperm activity. The period of use of a copper IUD is no more than 10 years.
- Hormonal IUD. After injection, it releases the hormone progesterone. This hormone is secreted daily, inhibits the maturation of the egg. You can use up to 5 years, then change the spiral.
In their appearance, both spirals from pregnancy look like the letter T, at the end of which there are two small antennae.
In addition to their main function, the uterine spirals protect against inflammatory diseases.
Indications
As noted above, the benefits of the spiral are not only in the inability to become pregnant. The spiral is shown to be installed for the treatment of various diseases, such as:
- Problems with menstruation. Painful, hard tolerable periods, irregular, etc .;
- pelvic pain;
- Uterine fibroids and endometriosis. Early endometrial cancer and precancerous condition;
The spiral produces a bactericidal effect, therefore, it alleviates the condition in case of illness and does not allow deterioration.
The intrauterine device is very indicated for women who have given birth, who do not have STDs and diseases of the cervix.
Various complications
The most frequent period after the installation of the IUD, when various complications appear, is the first three months.
Spiral drop. It is not necessarily accompanied by painful sensations and does not harm the body. Sometimes a woman does not notice at all that the spiral has fallen out. Loss can occur both immediately after the procedure, and for quite a long time after the introduction of the spiral. The reason for the prolapse of the IUD can be great physical exertion and deformation of the cervix. Also, if an incompetent doctor installed the helix incorrectly or chose an IUD that was not suitable in size and type for the body. Sometimes prolapse occurs for the harmless reason of rejection by the body of a foreign object. In this case, after getting used to everything passes.
Often in the first month after the procedure, girls experience a delay in menstruation. In this case, anti-inflammatory drugs are taken that normalize the cycle and protect against inflammatory processes in the uterus. Inflammation of the uterus is due to intolerance to the IUD, as a type of contraceptive.
With heavy and prolonged bleeding after the IUD insertion procedure, you need to urgently go to the hospital. The doctor prescribes tests and examinations. The first thing the doctor will pay attention to is whether the woman has gynecological diseases. If it does not stop, but there are no serious diseases, the spiral is removed, otherwise a complication may occur in the form. During treatment, the patient is regularly examined and monitored for the course of the disease.
To prevent symptoms, the doctor prescribes medications containing iron and recommends eating more foods that are rich in iron.

Other complications
Frequent complications from the beginning of the use of the IUD are heavy bleeding and loss of the spiral at different times. But there are other, rarer complications.
Most arise, as a rule, from a copper spiral.
- Too painful menstruation;
- pelvic infections;
- Damage to the uterus with a spiral;
- Irregular periods. Sometimes they disappear altogether;
- Ectopic pregnancy, miscarriage, subsequent early birth.
Infertility. It is because of this complication that doctors recommend using spirals only for women who have given birth.
Contraindications
Before installing the spiral, a woman needs to undergo a small examination and pass the tests prescribed by the doctor, because the IUD is not suitable for everyone, moreover, sometimes individual intolerance appears after the introduction.
It is impossible to install a spiral for oncological diseases of the genital organs, if a woman has cervical cancer, pelvic infections, cervical cancer, with uterine bleeding,. Also with deformation of the uterus and if there are sexually transmitted infections. It is forbidden to use the IUD for a woman if 3 months have not passed since the abortion and if the woman has had an ectopic pregnancy in the past.
An examination is necessary to identify possible problems and the doctor decided whether it is possible to put a spiral without harm to the woman's body.
Installation
Before you go to the very procedure for the introduction of the IUD, you need to carry out a number of preparatory measures: pass the tests that the doctor will prescribe, undergo an examination by a gynecologist and carry out the procedure.
Examinations to be completed before the procedure:
- pregnancy testing;
- Examination for STDs and other gynecological problems;
- and other types;
- The doctor must examine the genital organs: vagina, uterus, etc., and then selects the best type of IUD for a woman.
Before the procedure itself, the gynecologist measures the size and depth of the uterus. The process of installing an intrauterine device feels like inserting a speculum during an examination. There is no severe pain during the procedure, but there are unpleasant sensations. If a woman does not tolerate the slightest discomfort, the doctor may inject painkillers into the cervical region. Installation of the spiral takes 10 minutes.

Rehabilitation
After installing the intrauterine device, you need a sparing daily routine, more rest, you can’t strain yourself too much with work. The spiral for the body is a foreign object, it takes some time to get used to and the body experiences stress, so extra loads during rehabilitation will only aggravate the condition. The rehabilitation period after the installation of the spiral is different for all women. If there is no pain and heavy bleeding, you can perform the usual amount of work. Just do not forget that any overvoltage can cause disturbances, the most common of which is the loss of the spiral.
Since the prolapse of the spiral from the uterus of a woman most often occurs during the first 8 months, a verification procedure must be carried out. You can determine the position of the spiral by the antennae. You can check it yourself with your fingers, but if a woman cannot check it herself, you need to entrust the matter to a gynecologist. You need to be examined by a doctor monthly. Then the dangerous period will pass easily and without complications.
When to see a doctor
Small or meager daubing is a natural reaction of the body after the introduction of the spiral, as it occurs in almost all women. The average period is 6 months, but the time to stop the discharge is individual and can vary from 4 to 8 months. It happens that there are no discharges at all, but this is very rare and not dangerous.
Only prolonged and abundant discharge becomes dangerous. It looks like a period that hasn't stopped for several weeks. In case of heavy bleeding, you should immediately consult a doctor. Also, if the discharge goes long enough, it is better to visit the hospital, since heavy bleeding and smears for more than 8 months can be caused by serious disorders in the body.
Sometimes a spiral in a woman can provoke various diseases of the uterus, then bleeding signals inflammation. If the examination reveals a negative effect of the spiral, it is removed and no longer placed. In this case, other methods of protection are prescribed.
Using a spiral during breastfeeding
An IUD can only be inserted six weeks after delivery. The ions released by the intrauterine device penetrate the mother's blood, but harmful substances make up only one thousandth of a percent of the daily volume of mother's milk. This amount is too small to harm the health of the baby, so the use of the spiral during breastfeeding is safe for mother and child.
The need for removal
There are many reasons why it is necessary to remove the coil, or change it for a new one.
The need to remove the spiral may arise in the following cases:
- The hormonal intrauterine device must be changed after every five years of use, the copper one after ten years.
- When using other protection against pregnancy, you need to remove the coil at the beginning of the menstrual cycle.
- After removing the intrauterine device, the next installation is performed only after a month.
- If inflammation or infection has appeared due to the spiral, as well as with heavy bleeding, the spiral must be removed.
- With individual intolerance to the IUD. If, when using the IUD, a woman has a constant stomach ache in the uterus, or experiences discomfort, the spiral must be removed and another method of protection used.
Pregnancy with an intrauterine device
IUD is the most popular way to prevent unwanted pregnancy, not only because of the simplicity of the procedure, but also because of its excellent effectiveness. There is practically no chance of getting pregnant with an IUD. And yet, pregnancy with an intrauterine device is possible, although it is extremely rare and for certain reasons. For example, an incorrectly installed spiral, or jumped off during too passionate sexual intercourse.
To exclude such a pathology as an ectopic pregnancy, if you suspect a pregnancy, you should consult a doctor for examination. If the pregnancy proceeds normally, there are no complications, and the woman wishes to endure and give birth to a child, the coil is removed.
The doctor will remove the spiral without harm to the mother and child. But there are cases when, when the IUD is removed, the pregnancy is terminated.
If a woman does not trust doctors, the child can be carried without removing the intrauterine device from the uterus. But in this case, one must be mentally prepared for the fact that the development of the fetus will not go so smoothly, complications in the growth and development of the child are possible.
By the way, very few cases of successful gestation are known, along with an intrauterine device. But there is always a risk of pathologies for the child.
To avoid unpleasant consequences and make pregnancy comfortable and safe, it is necessary to remove the spiral. Or, if a woman does not want to give birth to a child, terminate the pregnancy, since the IUD and pregnancy cannot successfully exist simultaneously, and both mother and child may lose their health for delay.
The intrauterine device is one of the most effective methods of contraception exclusively for women. It is not possible to use it on your own, since a gynecologist should deal with its introduction. But before such a procedure, you must first undergo an appropriate examination in order to prevent possible complications.
Types of intrauterine device
To date, the 2 most common types of helix are known - hormone-containing IUD and copper IUD. Both of them look like the letter "T" with two small antennae at the end. The hormone-containing spiral after the introduction begins to release the hormone progesterone, the copper one, respectively, releases copper ions. The time of operation of the hormone-containing spiral should not exceed 5 years, and the copper one can be inside the uterus for 10 years.
There are opinions that after the removal of such a spiral, a woman will no longer be able to give birth. This is absolutely not the case, and to be more precise, it is not so for everyone. Many after the removal of the spiral become pregnant and give birth successfully. It is also worth noting that two types of spiral perfectly protect against sexually transmitted diseases.
In what cases it is necessary to install spirals?
All spiral settings are made purely to prevent unwanted pregnancy. But, despite this, these types of contraceptives can be installed for other purposes. Most often this occurs to treat diseases such as pelvic pain, precancerous conditions or already early endometrial cancer, heavy and painful menstruation. This rather short list of reasons why coils are installed at first may seem pointless. But this is absolutely not the case, because many women really cannot do without it, especially when it comes to a young girl with early problems of female function. After the installation of such a spiral, health improvement occurs.
Complications after IUD coil insertion
The most common occurrence of complications after installation is the loss of the spiral from the uterus. It is worth noting that such a phenomenon can occur not only immediately after it is introduced into the uterus, but also for three months after the procedure. The body gets used to the spiral and prolapse in some cases can be normal. We can say with confidence that it is during this period that complications of a different nature occur.
Uterine bleeding is another type of complication after the introduction of the spiral. As a rule, the problem is such if the blood flow is strong enough. Then the woman needs individual treatment, which is prescribed either after the removal of the spiral, or with its presence. If the spotting is not significant, then there is no cause for concern. After appropriate treatment, the coil must be removed if it does not have any contraceptive effect.
Today, another rather serious complication after the installation of an intrauterine device is known - this is perforation of the uterus. This complication appears quite rarely, but in case of it it is necessary to urgently treat. In the future, the use of a spiral after such a complication is categorically not recommended.
Why is there blood after the introduction of the spiral?
There is no cause for concern if, during the first six months after the introduction of the intrauterine device, there is light uterine bleeding or spotting. Such phenomena do not pose any danger to the health of a woman and may well be observed in every patient. You should only worry if the blood goes strong enough and for a long time. In this case, you need to consult a doctor for help, because self-medication will not help here.
Normally, light spotting should fade away, but if after eight months after the installation of the spiral they do not stop, you should consult a doctor. As for the issue of menstruation, then for their normalization, you can take special anti-inflammatory drugs. They will help not only restore the cycle, but also protect against unwanted inflammatory processes around the inserted coil in the uterus. Such inflammation also sometimes happens. Most often this is due to individual intolerance to this type of contraceptive.
What to do with severe bleeding after the installation of the spiral?
Most often, patients with severe bleeding after the installation of the spiral are prescribed special and regular monitoring for a certain time. The necessary tests are given and examined for the presence of possible gynecological diseases. If nothing special and serious is revealed, and the blood continues to flow strongly, then the spiral is removed. If this is not done, then cases of anemia in women are known as a complication. For the prevention of the disease, preparations containing iron and all kinds of food rich in iron are prescribed.
Other complications arising after the installation of the spiral
In addition to the fact that women often complain of bleeding after the introduction of the spiral, other side effects can be observed. These are cramps, severe pain during menstruation, the spiral falls out of the uterus, subsequent infertility, various pelvic infections, mechanical damage to the uterus during the installation of the spiral, irregular periods or their absence. Most often, complications of this nature occur after the installation of a copper spiral. If, during the presence of the spiral, a woman becomes pregnant, then it is more likely that this pregnancy is ectopic. Other problems may also occur, such as miscarriage, pelvic infections, and early labor.
It is worth noting that the intrauterine device is not suitable for all women. Therefore, before installing it, it is necessary to carefully check and pass all the necessary tests, and only after that decide on this procedure. We highlight the main cases when the use of a spiral is strictly prohibited:
- deformation of the uterus;
- vaginal bleeding of a different nature;
- the occurrence of an ectopic pregnancy by inheritance;
- had an abortion in the last three months or a pelvic infection;
- the presence of various sexually transmitted diseases;
- the presence of cervical cancer or cervical cancer;
All of the above problems must be detected and clarified during examination with a doctor, and only after that prepare for the installation of the spiral.

Spiral installation procedure
Before proceeding directly to the procedure, a woman must undergo an appropriate examination:
- pregnancy test and the presence of sexually transmitted diseases;
- examination of the uterus, vagina and other organs;
- the most appropriate type of intrauterine device for installation is determined.
Anesthesia is not used for this procedure. You can only use a special gel that will slightly anesthetize all the doctor's actions. In some cases, a special injection is made into the cervical region to reduce possible pain and discomfort. The introduction of the spiral itself resembles a regular examination by a gynecologist with a speculum. Only before direct installation, the doctor should measure the size of the uterus and its depth. The whole procedure takes no more than 10 minutes. This procedure does not cause much pain.
Only unpleasant sensations may be present during the introduction of the spiral, or after. If desired, in order to reduce unpleasant sensations, painkillers are administered to some patients.
What to do after installing the spiral?
Recovery after the introduction of the spiral may take some time. As a rule, every woman is different. As a generally accepted rule, it is recommended to rest more at first, not to exert yourself with physical exertion, especially if severe bleeding is observed. If nothing hurts and there is practically no bleeding, you can return to your normal work schedule. But remember, any voltage can lead to malfunction.
For the body, this is already a new phenomenon, and additional stress can only harm. For a certain time after a month, check with your fingers for the presence of antennae in the vagina. This will help to independently control the position of the spiral in the uterus. If you can not do it yourself, then visit the gynecologist every month for a check and an accurate result. In order for the recovery process to be successful, follow the instructions of the doctor as much as possible. in this case, the rehabilitation period will be successful.
When should you see a doctor for bleeding?
As mentioned above, spotting or light spotting during the first 4 months is normal. There are cases, of course, when this is not the case. But this is so rare that long-term discharges have become the norm. It is worth sounding the alarm only in cases where the blood goes too much and for a long time. It may look as if the period continues for several weeks. With such a diagnosis, it is imperative to go to the hospital for help to make sure that there are no serious violations or to stop them in time.
Quite often there are cases when bleeding is a signal of the presence of serious diseases, which provoked the introduction of the spiral. Then the IUD must be urgently removed and other possible methods of contraception prescribed.

Using a coil while breastfeeding
Scientists have found that it does not pose any danger to the baby. This can be explained by the fact that the substance of the IUD still penetrates into the blood plasma, but the harmful content is only 0.1% of the daily dose of excreted milk. Such an amount cannot harm the baby. Therefore, the use of the spiral after childbirth is quite safe for both the child and the mother. It is only worth remembering that the IUD must be installed six weeks after the birth of the child.
In what cases is it necessary to remove the spiral?
- After five years of use, in particular the hormonal intrauterine device. The copper coil must be removed after 10 years of successful use.
- Removal of the spiral with possible other contraceptives must be done at the beginning of the menstrual cycle.
- It is allowed to install a second spiral after a month after the removal of the previous IUD.
- In the presence of heavy bleeding for a long time.
- With constant pain in the lower abdomen and discomfort during intercourse. Perhaps the spiral is not suitable for you and it is better to choose another method of contraception.
 Does ureaplasma pass by itself (can it pass on its own)?
Does ureaplasma pass by itself (can it pass on its own)? PCR analysis to detect chlamydia Chlamydia PCR how to do
PCR analysis to detect chlamydia Chlamydia PCR how to do COCs with different daily dosages: how to choose, an overview of the best drugs
COCs with different daily dosages: how to choose, an overview of the best drugs Ureaplasma parvum: characteristics, tests, symptoms in women and men, what is dangerous, whether it is necessary to treat
Ureaplasma parvum: characteristics, tests, symptoms in women and men, what is dangerous, whether it is necessary to treat Basic technologies for obtaining nanomaterials
Basic technologies for obtaining nanomaterials How to tell the time in English?
How to tell the time in English?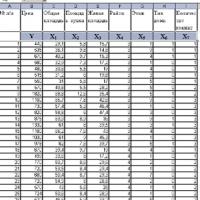 Introduction to Multivariate Statistical Analysis
Introduction to Multivariate Statistical Analysis