How does Ureaplasma spp. in men? Ureaplasma spp (ureaplasma spp) Ureaplasma spp in men
Under the name Ureaplasma species, two types of bacteria are combined: Ureaplasma urealyticum, Ureaplasma parvum. Their favorite habitat is the organs of the genitourinary system. Much less often, these microorganisms can be found in the lung tissue.
Ureaplasma spp was first identified by Shepard in 1954 in a patient with urethritis. Initially, these microorganisms were called T-mycoplasmas (from the word tiny, which means tiny in English). In the course of further research, it was found that up to 80% of sexually mature people with several partners are carriers of this microorganism.
The opinions of doctors about ureaplasmosis were divided. Many believe that treatment does not make sense, since Ureaplasma spp is an opportunistic pathogen, and if it does not cause unpleasant symptoms, then it is unnecessary to get rid of it.
There are several ways of infection with ureaplasma:

- Most often, Ureaplasma enters the body of an adult during unprotected intercourse (vaginal, anal, oral). The main carrier of the disease are women with severe symptoms of the disease, having more than two sexual partners per year. Males in most cases become temporary carriers, but during this period they can infect their partners.
- Ureaplasma can enter the body during transplantation of donor organs. In very rare cases, infection occurs during blood transfusion.
- Ureaplasma enters the uterus through the placenta, which can lead to inflammation of the walls of the fetal bladder or intrauterine infection of the fetus and subsequent congenital pneumonia in the baby.
- Also, a child can become infected with ureaplasmosis, passing through the birth canal of an infected mother. In 40% of children, Ureaplasma was detected in endotracheal secretions. The study was conducted within 24 hours after delivery.
You can not get infected with ureaplasma in a household way, through a bed or towels. It is also impossible to get a disease when visiting a sauna, bath, swimming pool, public toilet or while swimming in an open pond.
Disease Development Factors
Ureaplasma species is detected and begins to actively multiply, causing unpleasant symptoms in the following cases:
- Promiscuous sexual relations, and as a result - infection with other venereal diseases.
- Diseases that result in disorders of the immune system.
- Chronic inflammatory processes of the genitourinary system.
- Abuse of Miramistin or Chlorhexidine solutions, which are used to prevent infection with sexually transmitted diseases transmitted through unprotected intercourse.
- The use of antibiotics that do not affect ureaplasma, corticosteroids, oral contraceptives.
- Frequent stressful situations, hypothermia of the body.
- Pregnancy period.
- Chronic prostatitis in men.
- Damage to the mucous membrane of the urethra.
- High pH in the vagina in women.
Signs of the disease
Carriers of ureaplasma in most cases have no symptoms. Examination does not reveal pathology of the genitourinary tract. In smears from the urethra, vagina, cervical canal, the number of leukocytes is normal. The incubation period is about 19 days. After this period, the infection that has entered the body can reveal itself. If the prescription of the disease is more than two months, it is regarded as chronic.
In men
Often, ureaplasma spices, entering the body of a man, does not manifest itself in any way, and its presence can be determined only after passing the tests. But in the event that favorable conditions arise, it becomes the cause of diseases of the genitourinary system, accompanied by unpleasant symptoms.
Most often in women, Ureaplasma colonizes in the vagina without causing any symptoms. Sometimes these microorganisms settle in the uterus, which is more dangerous.
In most cases, Ureaplasma causes several gynecological and urological diseases that differ in their symptoms.
In 20% of cases, infection with Ureaplasma species can cause diseases of the pelvic organs. Such diseases include:
- Acute parametritis.
- Salpingitis and oophoritis.
- Endometritis.
In this case, pain occurs in the lower abdomen, the menstrual cycle fails, vaginal discharge and symptoms appear in the form of fever, chills, dizziness and headache. In women, joint damage is less common than in males.
Ureaplasma in pregnant women
During pregnancy, a woman's immunity does not work at full strength, which makes it possible for Ureaplasma to actively develop and cause unpleasant symptoms. In order to prevent this, it is necessary during the planning period to consult a gynecologist and treat ureaplasmosis.

In some cases, the appearance in the body of ureaplasma parvum or urealiticum can cause the following pathologies:
- If the infection occurred in the first trimester of pregnancy, then a miscarriage is possible.
- In late pregnancy, the development of cervical insufficiency and the threat of premature birth is possible (Ureaplasma urealyticum or parvum was detected in about 30% of women with this diagnosis).
- Postpartum endometritis (detected in 10% of women with ureaplasmosis).
- postpartum fever.
If intrauterine infection of the fetus occurs through the placenta or when passing through the birth canal, then this can provoke acute pneumonia, chronic lung disease, sepsis or meningitis. In some cases, ureaplasma can adversely affect the baby's nervous system, causing neurological diseases in him. Ureaplasma can also cause intrauterine death of the fetus.
Diagnostics
In order to diagnose the disease, the doctor conducts a survey of the patient. In the future, women are waiting for a gynecological examination and taking swabs from the vagina and cervical canal.
Men undergo an examination of the external genital organs, a rectal examination of the prostate, and palpation of the scrotum. Then urine, material from the urethra and seminal fluid are taken for analysis.
Visually diagnosing the infection will not succeed. In order to identify it, it is necessary to conduct a number of studies:
- Microbiological research. The material is taken from the mucous membrane of the urethra (depth 2-3 cm). It is placed in test tubes with a nutrient medium and incubated in a thermostat at a temperature of 37 degrees during the day. Then examined with a microscope.
- Polymerase chain reaction PCR. This method allows you to identify the DNA of ureaplasma. For research, material is taken from the urethra or vagina. The result of the analysis becomes known within 6-7 hours. The disadvantage of the method is that it does not make it possible to determine the amount and sensitivity of ureaplasma to antibiotics. Also, the PCR method gives a positive result within 2 weeks after the end of treatment.
- Linked immunosorbent assay. The material for analysis is blood from a vein. Using the serological method, antibodies to ureaplasma antigens can be detected. This method is used for infertility.
Many doctors say that a microbiological study does not always give an accurate result, since the amount of ureaplasma is determined not in the vagina or urethra, but on the surface of the probe or tampon. Also we are talking about the fact that the sensitivity to antibiotics in vitro and in the body is different. Therefore, the PCR method is preferred. It is a more sensitive, faster and more effective test for diagnosing a disease than microbiological testing.
Treatment
It is necessary to take medications for the treatment of ureaplasmosis in the following cases: the presence of unpleasant symptoms, the ureaplasma titer during the analysis is more than 104 CFU / ml, frequent miscarriages or the threat of premature birth, infertility, upcoming surgery on the genitourinary organs, pregnancy planning.

Both sexual partners need to be treated, since re-infection with ureaplasma is possible. While taking antibiotics, you should not drink alcoholic beverages, as this can cause serious side effects. For the period of their use, you need to abandon sexual contact.
A control bacteriological study in women is carried out one week after the end of the drug intake. And the PCR method can be applied after 14 days. In order to make sure that there is no ureaplasma in the body, control is carried out for 2 to 3 menstrual cycles. The material is taken 2 days after the end of menstruation. In males, the disease is considered cured if, four weeks after the end of treatment, Ureaplasma is not detected in smears.
In order to get rid of the disease, antibiotics and drugs are used to improve the functioning of the immune system. To choose a drug and a treatment regimen, it is necessary to conduct a laboratory study and identify the sensitivity of microorganisms to antibacterial agents. Many researchers argue that ureaplasma spp quickly acquires resistance to drugs.
macrolides
Azithromycin (Summamed, Clarithromycin, Vilprafen, Erythromycin) These drugs belong to the group of macrolides. They quickly and effectively help to cope with the disease.

In order to get rid of ureaplasma, they are prescribed as follows:
- Clarithromycin 500 mg daily. You need to take the drug for 1 to 2 weeks, dividing the daily dose into two doses.
- Vilprafen 1.5 g per day, divided into three doses for 7 to 14 days.
- Azithromycin 500 mg per day for 6 days or 1 g for three.
- Erythromycin 2 g per day, divided into four doses for two weeks.
Erythromycin and Vilprafen are used if ureaplasmosis is detected in pregnant women. This group of drugs is usually well tolerated, but in some cases may cause vomiting, nausea, indigestion or dizziness.
Tetracyclines
Doxycycline (Unidox Solutab, Vibramycin). The drugs belong to the group of tetracyclines. For the treatment of ureaplasmosis, 400 mg of the drug is taken on the first day, then the dose is reduced to 200 mg, divided into two doses. Treatment is continued for one or two weeks.

The drugs in this group effectively fight the disease. Very good results of their use in women with infertility. After taking them, they managed to get pregnant and give birth at term without complications. But you need to remember that approximately 33% of strains of ureaplasma spp are resistant to drugs in this group, so in some cases you need to choose other means.
When taking tetracyclines, there are often side effects from the digestive tract, in the form of nausea, vomiting, and flatulence. There have also been cases of photosensitivity of the skin. Preparations of this group are not recommended for the treatment of ureaplasmosis in pregnant women.
Fluoroquinolones
Ofloxacin (Taricin, Avelox, Pefloxacin). These drugs belong to the group of fluoroquinolones. They are well absorbed and in high concentrations are found in the tissues of the body, which allows you to quickly and effectively get rid of ureaplasma. In recent years, up to 30% of these microorganisms are not sensitive to tetracyclines and macrolides.

For the treatment of ureaplasma, drugs are used as follows:
- Ofloxacin 400 mg per day divided into two doses for one or two weeks.
- Pefloxacin 600 mg once a day for a week.
- Avelox 400 mg once a day for 10 days.
As well as tetracyclines, fluoroquinolones are not recommended for use during pregnancy and lactation. With their use, side effects from the gastrointestinal tract and photosensitivity may occur.
Immunotropic therapy
In order to get rid of ureaplasma, not only antibiotics are used. In order for the body to cope with the disease, drugs are prescribed that improve the functioning of the immune system. The most commonly used drugs are:

- Immunomax 200 U on the 1st, 3rd, 8th, 10th day of antibiotic treatment.
- Polyoxidonium 6 mg once a day for the first three days, then every other day. The course of treatment will require 5-10 injections.
- Likopid 10 mg once a day for two or three weeks.
In 70% of cases, Ureaplasma spp is not a monoinfection, but manifests itself against the background of other diseases. Therefore, in order to get rid of unpleasant symptoms, antiprotozoal drugs (Trichopolum, Metronidazole) and antifungal agents (Fluconazole, Nystatin) are used in combination with antibiotics.
For the treatment of ureaplasmosis in women, drugs in the form of suppositories can also be used. These funds include Terzhinan, Betadine, Hexicon. They are injected deep into the vagina once a day at bedtime. The course of treatment is from 7 to 10 days.
Folk methods
In addition to traditional methods of treatment, folk remedies are also used:
- Chamomile and calendula flowers are mixed in the same proportion. 5 g of raw materials are poured into 500 ml of boiling water and allowed to brew for an hour. Strain and use for douching and washing the genitals. Treatment is continued for 10 days.
- A small head of garlic is crushed, poured with 250 ml of warm water and allowed to stand for half an hour. Strain and use for douching. Procedures are carried out within a week.
- To treat the disease and maintain immunity, you need to eat 100 g of fresh cranberries daily or drink 50 ml of fresh juice. Treatment continues for a month.
Prevention
In order to avoid infection, the following recommendations must be followed:
- Observe the rules of personal hygiene.
- During sexual intercourse with unreliable or new partners (including oral), use condoms.
- If the condom breaks during intercourse, antiseptics such as Miramistin should be used.
- In order to strengthen the immune system, you need to eat right and exercise.
- It is necessary to treat all infectious diseases in time in order to prevent their transition to a chronic form.
At the first signs of ureaplasmosis, you need to seek the advice of a specialist.
Ureaplasma spp. – a normal inhabitant of the human body, inhabiting the mucous membranes of the genitourinary organs and causing inflammation of the urogenital tract with a decrease in immunity. When the number of microorganisms in the discharge of the genital organs and urethra exceeds a certain threshold, the disease begins to manifest clinically: women have symptoms of vulvovaginitis, and men have urethritis or prostatitis. After the detection of microbes, typing is carried out, during which the type of ureaplasmas and their number in the body are determined.
Ureaplasmosis is a ticking time bomb. This is an infectious disease transmitted mainly through sexual contact. Ureaplasmosis can be asymptomatic or manifest with pronounced clinical signs with each exacerbation. This is a rather unpleasant pathology, leading to a disorder of sexual function and infertility. Ureaplasma spp is considered a pathogenic and harmful to the body microbe, sexually transmitted.
In the absence of timely and adequate treatment, ureaplasmosis leads to the development of severe consequences: cystitis, arthritis, adhesions, infertility. The rate of development of these pathologies and complications has been growing rapidly in recent years. Ureaplasma spices often prevents couples from becoming parents.
Ureaplasma species
Ureaplasma spp is a gram-negative specific coccobacillus from the mycoplasma family, which is a transitional substance from a virus to a bacterium and does not have a cell wall. Ureaplasma got its name due to its ability to hydrolyze urea.
The favorite habitat of ureaplasma species is the urogenital area. In more rare cases, the microbe settles in the lung or kidney tissue. Ureaplasma spp is the common name for opportunistic microbes that have similar morphological and biochemical properties: ureaplasma urealiticum and ureaplasma parvum. The term "species" is used when PCR analysis reveals DNA structures characteristic of ureaplasma, without further research and determination of the type of ureaplasma.
Ureaplasma species can persist for quite a long time on the mucous membrane of the genital organs and does not manifest itself in any way. Often, carriers of the infection find out about this quite by accident during a physical examination. People live quietly with ureaplasma spp all their lives, unaware of their presence.
Under the influence of adverse factors, the natural balance of microorganisms in the body is disturbed, ureaplasmas begin to multiply intensively and manifest their pathogenic properties, causing various ailments.
Factors contributing to the infection of ureaplasma species:
- Changes in the intestinal microflora,
- Decreased leukocytes in the blood
- Deterioration of the skin
- Immunodeficiencies,
- Chronic diseases of the urinary organs,
- Abuse of local antiseptics,
- Acid-base imbalance in the woman's vagina,
- bacterial vaginosis,
- STI,
- Taking antibiotics and hormones
- Injuries of the genitourinary organs,
- frequent stress,
- hypothermia,
- Pregnancy, childbirth.
Ureaplasma spp is dangerous because it passes through micropores and is resistant to a number of antimicrobial drugs. The bacterium invades the genome of germ cells and disrupts their functions.
Epidemiology
The source and reservoir of infection are sick women and persistent carriers of ureaplasmas. Men are considered temporary carriers of the infection, capable of infecting women during intercourse.
Infection with ureaplasma spp. happens in several ways:
- Sexual - with oral-genital, vaginal and anal contact,
- Vertical - from a sick mother to a fetus during pregnancy and childbirth,
- Hematogenous - through an infected placenta and umbilical cord vessels,
- Transplantation - in organ transplantation,
- Hemotransfusion - with blood transfusion,
- Contact household - in extremely rare cases.
Sexual transmission of infection is most common. Infection usually occurs during unprotected intercourse. Since ureaplasmas are very small microorganisms, they can freely penetrate even through the pores of a condom. In people with strong immunity, pathology develops extremely rarely.
Ureaplasma spp is most often found in women who have several sexual partners, who are preparing to become a mother, undergoing hormone therapy, and in socially disadvantaged individuals.
Symptoms
In healthy people, ureaplasma spp does not manifest itself in any way. At the slightest malfunction in the body, immune defenses decrease, and clinical signs of ureaplasmosis appear.

In men, ureaplasmosis usually proceeds as urethritis, epididymitis, cystitis, pyelonephritis. Ureaplasma species nest in women in the vagina and in the uterine cavity. It causes vaginitis, cervicitis, endometritis, cervical neoplasia, cervical insufficiency, urethral syndrome, and urinary incontinence. Pre- and postmenstrual periods are the most suitable time for the appearance of clinical signs of the disease. The younger the woman, the more pronounced the symptoms of ureaplasmosis.
Clinical signs of diseases caused by ureaplasma species:
- Women have mild vaginal discharge without color and odor, sometimes with an admixture of blood; pain in the lower abdomen, aggravated during intercourse and immediately after it; itching and burning in the perineum; feeling of overflow of the bladder and other dysuric symptoms. Their libido decreases, and pregnancy does not occur for a long time. The mucous membrane of the cervix during examination is hyperemic and edematous.
- Men complain of cloudy, odorless discharge from the urethra that occurs in the morning; itching and burning in the perineum; lower abdominal pain; discomfort when urinating; soreness when touching the scrotum and head of the penis; decreased libido. In a man with ureaplasma, erectile dysfunction occurs, the consistency of sperm changes, sperm motility worsens, and their destruction occurs. Spermatogenic cells are deformed, sperm fluidity deteriorates.
These are symptoms of an acute form of pathology. In the absence of timely and adequate therapy, they gradually subside, the disease passes first into a subacute, and then into a chronic form. Patients have only a slight burning sensation and discomfort in the urethra and genitals. Patients often don't notice "mild" symptoms and trigger an infection. If the disease is not treated, adhesions may appear in the pelvic organs, narrowing the lumen of the fallopian tubes and blocking the seminal duct. Often the disease spreads up the urinary-genital tract.
Infected pregnant women often do not bear a child, they go into premature labor and are at increased risk of developing postpartum endometritis. If intrauterine infection of the fetus occurs, the newborn may develop pneumonia, malnutrition, and neuropathy.
Diagnostics

Diagnosis of ureaplasma infection in men begins with an external examination of the genital organs, palpation of the scrotum, rectal examination of the prostate. Then a smear from the urethra, urine and seminal fluid are taken from the patient and a microscopic examination is performed. Ultrasound of the prostate and scrotum allows you to confirm or refute the alleged diagnosis. In women, the vagina and cervix are examined, the ovaries are palpated, and a complete gynecological examination is performed. Microscopy of smears from the urethra, vagina and cervix, as well as ultrasound of the pelvic organs are additional diagnostic methods.
Laboratory diagnosis of diseases caused by ureaplasma species:

During the treatment of ureaplasma infection, patients are advised to give up sexual activity, adhere to a certain diet, and not drink alcohol. Two weeks after the therapeutic course, control of cure is performed.
- Antibiotic therapy is the main method of treatment for diseases caused by ureaplasma species. Patients are prescribed antibiotics from the macrolide group - Azithromycin, Sumamed, fluoroquinolones - Suprax, Cifran.
- Immunomodulators are used to increase immune protection - "Polyoxidonium", "Amiksin", "Likopid", "Immunomax".
- Antiprotozoal and antifungal drugs are used to prevent candidiasis - Metronidazole, Fluconazole, Itraconazole, Nystatin.
- Enzyme therapy and vitamin therapy.
- Diet therapy - exclusion from the diet of spicy, salty and any other irritating food.
- For the treatment of pregnant women, immunoglobulins are administered intravenously and ozone therapy is carried out.
The course of treatment lasts an average of two months. The indicator of cure is a negative result of PCR diagnostics, indicating the complete destruction of microbes in the test sample. With a more severe damage to the body, treatment can be extended up to six months. A control analysis for the presence of ureaplasma spp is carried out after 2 weeks and a month after the end of treatment.
Ureaplasma species is the causative agent of urogenital infection, resistant to a wide range of antibiotics and does not cause persistent immunity after treatment, which is associated with frequent relapses of the disease.
Prevention
Preventive measures to prevent the development of ureaplasmosis:
- condom use,
- Treatment of the genital organs after sex with antiseptics,
- Hygiene of the genitals,
- Periodic testing for STIs,
- Regular visits to the gynecologist and urologist,
- Treatment of chronic diseases of the urogenital area,
- Maintaining a healthy lifestyle
- Strengthening immunity.
Ureaplasma species is present in the body of almost every person and quietly coexists with other bacteria without causing harm. But this does not mean that you can not pay attention to such “roommates”. The slightest excess of the allowable amount of these microbes often leads to the development of an individual reaction on the part of the body and causes various diseases.
Ureaplasma spices causes pathology in both sexual partners. Each of them should visit a doctor, undergo a diagnostic examination, based on the results of which intensive therapy will be prescribed.
Video: doctor about ureaplasma infection
Video: expert opinion on ureaplasma infection
One of the most common latent infections is ureaplasma species (ureaplasma spices). When infected, a person may not experience much discomfort and lead a normal life, infecting his partners. With a long course of ureaplasma spp in women, it causes inflammatory diseases of the reproductive organs and can cause infertility, miscarriages and birth complications. The pathogen can be detected using laboratory tests. Treatment is long and is carried out with antibiotics.
IT'S IMPORTANT TO KNOW! Fortuneteller Baba Nina:“There will always be plenty of money if you put it under your pillow…” Read more >>
1 What is ureaplasma
The microorganism belongs to non-gonococcal pathogens, which makes it especially dangerous for the urethra. The disease that it provokes - ureaplasmosis - is common and is diagnosed in about 1/3 of people with inflammatory pathologies of the reproductive organs. In order for such a diagnosis to be made, the analyzes should not reveal other pathogens of sexually transmitted diseases.
In the 70s of the 20th century, ureaplasma was considered an opportunistic microorganism that may be present in the microflora of healthy women, so no treatment was carried out. Modern Russian medicine, based on long-term studies, has come to the conclusion that this disease must be eliminated, especially when planning children.
Colonization of ureaplasmas causes a number of diseases of the genitourinary system:
Ureaplasma is often found in women with cervical insufficiency, pathologies during pregnancy and endometritis. In rare cases, this microorganism leads to infertility.
Symptoms, diagnosis and treatment of latent infections in women
2 reasons
The main cause of infection is sexual intercourse with an infected partner. This microorganism easily attaches to cells and spermatozoa and can enter the upper urogenital system of a woman. Due to its microscopic size, it is able to freely penetrate even through the pores of a condom.
The disease is transmitted from a sick woman to the fetus during pregnancy and childbirth. In 30% of newborn girls whose mothers are infected with ureaplasma, bacteria are detected in the vagina and nasopharynx. There is a low risk of exposure through household exposure, such as in a public toilet or visiting a contaminated swimming pool.
Pathogenic bacteria live on the mucous membranes - in the genital area and in rare cases - in the nasopharynx, lung and liver tissue. Therefore, a kiss is enough for infection. The following reasons may contribute to infection:
- Early onset of sexual activity.
- Frequent change of sexual partners.
- Taking hormonal drugs.
- Reduced immunity.
- Abuse of local antiseptics.
- Hypothermia.
- Previously transferred sexually transmitted diseases.
You can become infected with ureaplasma through blood transfusion and organ transplantation, but the main route of transmission of infection is sexual intercourse.
Ureaplasma in women: causes, clinic, diagnosis and treatment
3 Symptoms
Ureaplasma rarely manifests itself immediately after it enters the body. Usually, the first symptoms can be noticed only with a decrease in immunity and hormonal disruptions, when the disease is already becoming chronic. The classic signs of infection are:
- Cloudy and mucous discharge from the vagina.
- Drawing pains in the lower abdomen.
- Swelling of the genitals.
- Pain when urinating.
- Brown highlights.
- Burning when emptying the bladder.
- Discomfort during intercourse.
Women suffering from ureaplasmosis complain of vaginal discharge and pain. This symptom is characteristic of many sexually transmitted diseases and inflammatory non-infectious pathologies of the genitourinary system. In some women, ureaplasma does not manifest itself in any way, but they remain a source of infection.
Symptoms of trichomoniasis in women, diagnosis and treatment of the disease
4 Diagnostics
To detect ureaplasma, several tests are performed.:
- Polymerase chain reaction, or PCR (PCR, or polymerase chain reaction).
- Cultural research.
- Linked immunosorbent assay.
PCR diagnostics allows you to identify the DNA of the pathogen in the test material, which is usually discharged from the genital organs (scraping from the cervical canal, urethra, vaginal walls). Women are recommended to conduct such an analysis before menstruation or 2 days after it. A positive test result indicates the presence of uroplasmic infection. Negative - does not exclude the presence of the pathogen, but indicates its absence in the material.
A culture study is carried out with a positive result of PCR diagnostics to determine the total amount of the microorganism and its sensitivity to antibiotics. The analysis involves placing the biomaterial in a special nutrient medium, where active growth of ureaplasma is possible. The disadvantage of bacterial culture is its duration - about 8 days. When deciphering, 10 to the 4th degree CFU / ml is considered the norm.
ELISA determines the presence of antibodies in the body to a particular pathogen and the titer of detected bacteria. The test material is blood, which is placed on a special strip with antigens. One day is usually sufficient to obtain data, but the body does not always produce antibodies, so even if an infection is present, the result may be negative. The norm is a negative result.
If the patient complains of itching and burning in the genital area, the doctor prescribes additional examinations - urinalysis, ultrasound of the pelvic organs, microscopic examination of the microflora. This will identify other diseases that have developed against the background of ureaplasmosis.
5 Ureaplasmosis during pregnancy
During pregnancy planning, women are advised to take all tests for genital infections. Many neglect this procedure and find out about the presence of ureaplasma during the period of bearing a child. In this case, mandatory treatment is required, since the infection can be transmitted to the fetus. If in pregnant women ureaplasmosis is the cause of inflammatory pathologies of the reproductive organs, then in a newborn it can lead to the following diseases:
- Acute pneumonia.
- Blood poisoning (in rare cases).
- Meningitis.
- bronchopulmonary dysplasia.
Ureaplasmosis can be the main cause of ectopic pregnancy, premature birth, postpartum endometritis, miscarriage. To prevent this from happening, immediate treatment is required, and with a large amount of ureaplasma in the body, it is prescribed regardless of the period.
6 Treatment
Ureaplasmosis is treated with antibiotics. This microorganism is insensitive to penicillins and cephalosporins, so doxycycline and macrolides are the drugs of choice, which include:
- Azithromycin.
- Clarithromycin.
- Josamycin.
- Roxithromycin.
If ureaplasmas are resistant to these drugs, treatment is carried out with the help of fluoroquinolone antibiotics - Ofloxacin and Levofloxacin. During pregnancy, therapy is carried out with macrolides (Josamycin), starting no earlier than the 2nd trimester. If the disease is chronic, the doctor prescribes 2-3 antibiotics, and the duration of treatment reaches several months.
Therapy regimens may include antibacterial suppositories or douching solutions. With a decrease in immunity, immunomodulators are prescribed - Cycloferon or Viferon. With a long course of infection, enzymes are shown to prevent the formation of adhesions in the pelvis - Longidaza, Wobenzym.
The average duration of the course of treatment is 20 days. During therapy, it is important to follow a diet and give up salty, fried, spicy and smoked foods, alcohol. Sexual contacts are forbidden. After the end of the course, at least a month later, the woman needs to be re-examined. If ureaplasma is detected again during PCR diagnostics, a new therapy regimen is selected.
Treatment of ureaplasmosis is a long and expensive process, and after 20 days of taking antibiotics, PCR very often fixes a different form of the microorganism, which requires re-administration of drugs.
Urinary tract infections always require comprehensive and timely treatment, as they are prone to frequent relapses. The third most common among diseases of the genitourinary system is ureaplasmosis, second only to cystitis and pyelonephritis (inflammation of the bladder and renal pelvis). Ureaplasmosis is a predominantly acute inflammation of the walls of the urethra and mucous membranes lining the urethra. Pathology is caused by a bacterium from the group of opportunistic microorganisms - Ureaplasma urealyticum.
Ureaplasmosis
Scientists have several varieties of ureaplasma, but the most insidious is ureaplasma spices (ureaplasma spp). Infection with this bacterium is difficult to detect clinically, since inflammation is often asymptomatic, which distinguishes ureaplasma spp from other microorganisms of this opportunistic group. The disease is often “disguised” as other urinary tract symptoms and even sexually transmitted diseases, so it is almost impossible to diagnose ureaplasma spp at an early stage.
Ureaplasma spp
Causes of infection and risk factors
Ureaplasma spp is a normal inhabitant of the mucous membranes of the organs of the genitourinary system and is present in the human body throughout his life. The bacterium does not have a cell wall, so it is quite resistant to the effects of antibacterial drugs and antimicrobial agents. The microbe can exist on the mucous membranes of the bladder, urethra, ureters. A large number of ureaplasmas can be found on the surface of the genital organs, kidneys. In rare cases (mainly with a protracted course of ureaplasmosis), the bacterium can seed the epithelial membranes of the bronchopulmonary tissue, liver and intestines. Symptoms in this case can be blurred, so self-medication in the event of pathological signs from these organs is impossible.
Ureaplasmosis in women
The pathogenic activity of ureaplasma spp manifests itself when conditions favorable for its reproduction are created. In small quantities, this microbe is always in a latent state, and its activity is suppressed by cells of the immune system, but with a decrease in immunity, the number of bacterial colonies increases rapidly, and the body cannot produce enough immunoglobulins to fight the infection.
Analysis for ureaplasma - transcript
Experts consider the reasons and adverse factors for the development of asymptomatic ureaplasmosis:
- various types of addictions to substances with increased toxicity (tobacco and alcohol addiction, substance abuse, drug addiction);
- unreasonable intake of potent drugs and drugs containing hormones (usually this situation occurs during self-medication);
- a state of chronic stress, which can be provoked by a tense psychological situation in the family or at work;
- chronic diseases of the genital organs, urinary tract and venereal diseases;
- hypothermia;
- malnutrition, lack of regimen and activities aimed at strengthening the immune system (hardening, gymnastics, massage).
Smoking is one of the possible reasons
In women, frequent douching, especially with the use of antiseptic solutions, can provoke a decrease in local immunity. Washing with ordinary soap, the use of products that are not intended for the care of the intimate area, the use of pads with fragrances and coloring additives - all this negatively affects the vaginal microflora and can contribute to the creation of favorable conditions for reproduction.
Note! Pregnancy and childbirth are factors that provoke a natural decrease in immunity, including local immunity of the vagina and genitourinary tract, so ureaplasmosis during pregnancy is detected in every sixth woman, and after the birth of a child - in every fourth woman.
Ureaplasma spices in women
Ways of infection
Almost 80% of cases of infection with ureaplasma spp occur during sexual intercourse. A feature of this type of mycoplasmal bacteria is a very small size, so in some cases they can penetrate into the partner's genital tract even through the pores of condoms. If a person has strong immunity, infection will not occur, and microbes will not rise up the urinary tract, but if the protective functions are weakened, inflammation of the urethra or other organs of the genitourinary system will occur.
In most cases, infection occurs during sexual contact.
Ureaplasmas are usually not transmitted by household or contact routes, but doctors cannot exclude this method by 100%, since there are cases when, even in the absence of sexual contact, infection occurred (mainly when using personal hygiene items, dishes and other things belonging to the patient) .
Important! You can become infected with ureaplasma during a transfusion of donor blood, surgery or transplantation of internal organs, therefore, after such operations, the patient also needs constant monitoring and medical supervision for at least 30 days.
You can also get infected during a blood transfusion.
Ureaplasma spp during pregnancy
Ureaplasmosis during pregnancy is dangerous not only with possible complications (for example, glomerulonephritis and inflammation of the bladder), but also with a high probability of infection of the fetus and newborn. Bacteria can enter fetal tissues through the mother's systemic circulation, blood vessels, and infected placenta. The risk of infection also exists during the passage of the child through the birth canal, therefore, all women 2-4 weeks before the birth must pass a smear on the flora and undergo sanitation of the vaginal tract.
Molecular biological study on Ureaplasma spp
The consequences of infection with ureaplasma for a child can be:
- heart defects;
- blood disorders (including anemia and leukocytosis);
- congenital defects in appearance ("cleft palate", "cleft lip");
- severe disorders in the work of the digestive system;
- abnormal development of the organs of the genitourinary system.
Note! Newborns infected with ureaplasma have problems with sleep and appetite from the first days of life, so such children must undergo a complete medical examination to diagnose possible pathologies.
Examination by a gynecologist
Symptoms: how to recognize the disease in an asymptomatic course?
Untimely treatment of acute ureaplasmosis often leads to the transition of the disease into a chronic form, so it is important to consult a doctor if any signs of a possible infection are found. The danger of ureaplasma spp is that infection does not manifest itself with symptoms typical of ureaplasmosis, “masquerading” as other diseases and pathologies.
In women, pathology may have the following symptoms:
- hyperemia and swelling of the cervix (detected during examination by a gynecologist);
- a feeling of overcrowding of the bladder, accompanied by frequent urge to urinate with little urine output (about 5-30 ml at a time);
- burning in the groin and vaginal tract;
- soreness during sexual intimacy;
- drawing or dull pain in the lower abdomen.
Stomach ache
All these signs are characteristic only for the acute period. If at this stage the woman does not take any measures to fight the infection, the disease becomes chronic. Chronic ureaplasmosis is characterized by a slight burning sensation that occurs periodically (mainly with poor intimate hygiene or after emptying the bladder / intestines), and discomfort during sexual intercourse. If the infection has spread to the endometrium of the uterus, signs of endometritis and endometriosis may appear: intermenstrual bleeding, severe pain in the lower abdomen, fever.
In men, the clinical picture of chronic infection with ureaplasma spp is also erased, but with a careful attitude to one's own body, one can still notice the symptoms of an existing pathology. These may be atypical discharge from the penis, soreness of the penis, swelling of the prostate gland. Seminal fluid becomes less fluid, may smell bad, and its amount also decreases. The chemical composition of sperm also changes, as well as the number of active spermatozoa, which is easily diagnosed using a spermogram.
Clinic of ureaplasmosis in men
Important! Infertility can be an indirect symptom of ureaplasma infection, so partners who want to have children should be carefully checked for genitourinary infections in the absence of pregnancy during the year of regular sexual intercourse without the use of condoms and other means of protection. In women, ureaplasmosis can cause miscarriages, fading pregnancy or premature onset of labor, so even single cases of unfavorable gestation also require careful medical supervision.
Infertility is one of the indirect signs of infection with ureaplasma
What to treat?
The main drug group used for the treatment of ureaplasmosis are antibacterial agents that are active against gram-negative bacteria of the species Ureaplasma urealyticum. Penicillin drugs, which are the drugs of choice for the treatment of most genitourinary infections, are ineffective in combating ureaplasma spp, so doctors usually prescribe drugs from the group of fluoroquinolones, macrolides, and cephalosporins. The most effective drugs and an approximate dosing regimen are listed in the table.
Table. Antibiotics for the treatment of infections caused by ureaplasma spp.
"Supraks"
If secondary infection with fungi of the Candida family (urogenital candidiasis) is suspected, antimycotic agents of local or systemic action can be used. The most effective are the tablets "Fluconazole" and "Miconazole". For local therapy, antifungal agents with a wide spectrum of activity are used in the form of vaginal suppositories, capsules and tablets, as well as creams and ointments (Terzhinan, Vagisept, Pimafutsin).
"Terzhinan" (tablets for vaginal use)
With frequent relapses and a persistent decrease in immunity, the use of immunomodulators, for example, Polyoxidonium, is indicated. This is an immunostimulant in the form of suppositories for vaginal or rectal administration, as well as tablets for internal use based on azoximer bromide. In severe cases, a lyophilizate is used to prepare a solution that is injected.
"Polyoxidonium"
It is necessary to use "Polyoxidonium" for the treatment of ureaplasma infection according to the following scheme:
- 1 tablet 2 times a day half an hour before meals for 3-4 months;
- 6-12 mg, previously dissolved in 2-4 ml of sodium chloride solution 0.9%, intramuscularly 1 time per day (1-2 times per week);
- 1 suppository into the vagina or rectum 1 time per day at bedtime (before inserting into the rectum it is recommended to clean the intestines).
For treatment to be effective, both partners must undergo therapy. If a person is promiscuous, all sexual contact should be protected by condoms.
You must use condoms during sex
Of great importance in the treatment and prevention of ureaplasmosis is the state of the immune system, therefore, measures aimed at stimulating the activity of immune cells are one of the main directions in the complex treatment of infections caused by ureaplasma sp.
Video - Ureaplasma
Kind of weird. All my life I have been tested for infections (chlomidia, ureaplasma, mekaplasma). About five years ago, ureaplasma was found and cured. Then everything is always ok. Before last B handed over too, found nothing. After a miscarriage, everything is also clean. And then she came to G, she tells me, they say, last time you and I handed over the total ureaplasma, and now let's take it for all 3 of its types. And here is the result: Ureaplasma ur.T-960 - not detected, Ureaplasma parvum - detected, Ureaplasma spp - detected. What is this news? Which one did I have before...
Anonymously
Good day!
A week before the last menstruation, she took smears, Candida albicans (scraping), Gardnerella vaginalis (scraping), Ureaplasma spp. , I didn’t have time to go to the doctor, yesterday I found out about a new pregnancy (second), is it possible to have some kind of treatment, my first baby and I are still at guards!
Vaginal discharge and smear are normal
Vaginal discharge and smear normal All you read in women's letters is about doctors' fascination with the treatment of white blood cells in the vagina, because there is an opinion that white blood cells are a sign of inflammation. Is it so? Far from it! Leukocytosis plays a huge role in the reproductive function of a woman, including during pregnancy. We'll talk about this a little later. The amount of vaginal discharge Most women do not know what and how much vaginal discharge should be normal. This leads to...
Ureaplasmosis - symptoms and treatment
What is ureaplasmosis? We will analyze the causes of occurrence, diagnosis and treatment methods in the article of Dr. V. P. Kovalyk, a urologist with an experience of 25 years.
Definition of disease. Causes of the disease
Ureaplasmosis- a group of inflammatory and dysbiotic diseases associated with ureaplasmas ( Ureaplasma species). Since 1995, two types of ureaplasmas have been distinguished: Ureaplasma urealyticum and Ureaplasma parvum. Genome U. urealyticum much bigger U.parvum. At present, it is impossible to state that any of the species is an obvious pathogen or vice versa - a saprophyte.
Ureaplasmas are conditionally pathogenic microorganisms that are often found on the mucous membranes of the genitourinary organs, upper respiratory tract and in the oropharynx.
For the first time, ureaplasmas were isolated in the USA from a dark-skinned patient with non-gonococcal urethritis in 1954.
The first hit of ureaplasmas in the male urethra, as a rule, causes urethritis - inflammation of the urethra. There is evidence that in women, ureaplasmas are associated with acute pelvic inflammatory disease (PID), as well as with bacterial vaginosis. The role of ureaplasmas in the occurrence of bronchopulmonary diseases in newborns (bronchitis, pneumonia) and postpartum chorionamnionitis has been proven.
The role of ureaplasmas in human pathology has not been fully established. The study of the pathogenetic relationship of these microorganisms with a wide range of diseases from different areas continues:
Ureaplasmas are often part of the normal microflora of the urethra and vagina. The frequency of detection of ureaplasmas averages 40% in the genitourinary organs in women and 5-15% in men. Wherein U.parvum found much more frequently than U. urealyticum(38% versus 9%).
Ureaplasmas are spread through sexual contact. The more sexual partners during a lifetime, the more often the colonization of the vagina or urethra by ureaplasmas. Ureaplasmas are transmitted to newborns when passing through the birth canal. In this case, the colonization of the mucosa of the vulva and vagina in girls and the nasopharynx in both sexes occurs. The frequency of detection of ureaplasmas in newborns can reach 30% or more, decreasing to a few percent by the first year of life.
Subsequently, an increase in the frequency of colonization by ureaplasmas begins from the moment of the onset of sexual activity (at 14-18 years).
If you experience similar symptoms, consult your doctor. Do not self-medicate - it is dangerous for your health!
Symptoms of ureaplasmosis
Symptoms vary depending on the underlying disease.
Urethritis can be manifested by scanty discharge and burning in the urethra, frequent urination. Without treatment, urethritis tends to resolve itself: the symptoms subside, the patient calms down. Past urethritis increases the likelihood of future inflammation of the prostate gland - prostatitis. In addition, complications of urethritis can be epididymo-orchitis - inflammation of the testicle and its epididymis, vesiculitis - of the seminal vesicle and, rarely, cooperitis - of the bulbourethral gland.
Acute salpingoophoritis, endometritis can be manifested by pulling pains in the lower abdomen, fever, weakness and discharge from the vagina. Inflammatory diseases of the pelvic organs in women are a natural consequence of bacterial vaginosis observed when ureaplasmas are detected. Symptoms of the disease can quickly worsen, often requiring hospitalization in a gynecological hospital.
In addition to inflammatory diseases, ureaplasmas, in addition to many other microorganisms, are associated with bacterial vaginosis.
bacterial vaginosis, as a rule, it is accompanied by discharge with an unpleasant odor, which, moreover, increases during intimacy.
The disease predisposes to obstetric and gynecological complications: premature birth, low birth weight.
The author of the article shares the views of world experts in the field of urogenital pathology ( Jenny Marazzo, Jorma Paavonen, Sharon Hillier, Gilbert Donders) on the lack of connection of ureaplasmas with the occurrence of cervicitis and vaginitis.
It should be noted here that the Russian guideline calls for the treatment of cervicitis and vaginitis, based on the etiological role of ureaplasmas in these diseases, which, of course, is a mistake.
The pathogenesis of ureaplasmosis
Ureaplasmas are conditionally pathogenic microorganisms, that is, their pathogenic properties are realized only under special conditions: high concentration on the mucosa, immunosuppression, and others.
Ureaplasmas are attached to the surface of the mucous membrane with the help of cytoadhesin proteins. In addition to the urethral epithelium, ureaplasmas are able to attach to erythrocytes and spermatozoa.
One of the main factors of pathogenicity are the enzymes phospholipase A and C, under the influence of which prostaglandin is produced in the body - a factor that triggers contractions of involuntary muscles, therefore, premature birth is possible. The inflammatory response is accompanied by the production of pro-inflammatory cytokines - IL 6, 8, 10.

Ureaplasmas have IgA-protease activity, destroying the local protective factor of the mucous membrane immunoglobulin A.
The inflammatory process in the urethra develops with a high concentration of ureaplasmas. So it is shown that 10 3 CFU / ml and above is associated with the detection of 12 or more leukocytes per ml in the urethral contents.
Special factors of pathogenesis are realized when bacterial vaginosis occurs. At the same time, the factors of local mucosal immunity are weakened, due to which such patients are more susceptible to infection with sexually transmitted infections (including HIV). The acidity of the vaginal contents (pH is normal 3.5-4.5) is reduced to a neutral environment (pH 6.5-7 and above). Thus, the natural protective barrier against pathogens is weakened.
Classification and stages of development of ureaplasmosis
According to the duration of the course, they distinguish spicy and chronic urethritis. Acute urethritis - up to 2 months, chronic - more than 2 months. In the latter case, one distinguishes recurrent and persistent urethritis.
Chronic recurrent urethritis a disease is considered in which leukocytes in the urethra returned to normal by the end of treatment, and after 3 months their rise was again observed over 5 in the field of view (with an increase of x1000). Chronic persistent urethritis- when an increased content of leukocytes was observed at the end of treatment and after 3 months.
PID involves the fallopian tubes, ovary, and their ligaments being involved in the process. Inflammation of the appendages can be unilateral or bilateral, acute or chronic. The main symptoms: pain in the lower abdomen, in the lower back, discharge from the genital organs, temperature of 38 ° C and above.
Complications of ureaplasmosis
In men, complications of urethritis are balanoposthitis - inflammation of the head and foreskin of the penis. Prostatitis is also possible, less often - epididymo-orchitis and cervical cystitis. At the same time, ureaplasmas are not considered as an independent agent that causes inflammation of the prostate gland. Probably, this chain of complications occurs through posterior urethritis and is realized with the help of urethroprostatic reflux, i.e., reflux of the contents of the posterior urethra into the prostate acini and vas deferens.
In women, PID may be complicated by tubo-ovarian abscess, and occasionally peritonitis and sepsis occur. In the long term, serious complications are possible that have social consequences: chronic pelvic pain, and infertility.
It is unlikely that only the presence of ureaplasmas in the vaginal biocenosis will lead to such complications. These microorganisms realize their pathogenic potential together with other microorganisms, leading to dysbiotic changes - bacterial vaginosis.
Diagnosis of ureaplasmosis
Indications for the appointment of studies to identify ureaplasmas are clinical and / or laboratory signs of an inflammatory process: urethritis, PID. Routine studies should not be performed on all patients, incl. without signs of any disease.
To detect ureaplasmas, only direct detection methods are used: bacteriological and molecular genetic. Determination of antibodies: IgG, IgA, IgM is not informative. The material for the study can be the discharge of the genitourinary organs, urine, vaginal secretions, etc.
Bacterial vaginosis is verified using the Amsel criteria:
- creamy discharge on the walls of the vagina with an unpleasant odor;
- positive amine test (increased "fishy" smell when 10% KOH is added to the vaginal secretion);
- an increase in the pH of the vaginal contents above 4.5;
- the presence of key cells on microscopy of vaginal contents.

In the presence of any 3 of the 4 criteria, the diagnosis is established. However, due to the complexity of implementation, the impossibility of measuring pH, the evaluation of the Amsel criteria is difficult. There are commercial research panels based on quantitative molecular genetic methods ("Florocenosis", "Inbioflor", "Femoflor"), which determine the diagnosis of "bacterial vaginosis".
Treatment of ureaplasmosis
Treatment is indicated only in cases where, as a result of the examination, an obvious connection between ureaplasmas and the inflammatory process was revealed. In the case of a healthy carriage of ureaplasmas, treatment is not indicated. It is a vicious practice to prescribe therapy to all persons who have ureaplasmas.
Treatment is indicated for sperm donors and infertility, when no other causes have been identified.
Recent bacteriological studies have shown high activity against ureaplasmas of doxycycline, josamycin and a number of other antimicrobial drugs.
- Doxycycline monohydrate 100 mg 1 tab. 2 times a day;
- or Josamycin 500 mg 1 tab. 3 times a day.
With the persistence of the inflammatory process, the course can be extended up to 14 days.
When bacterial vaginosis is detected, vaginal preparations are prescribed:
It is important to note that the goal of treatment is not to "cure ureaplasmas", complete eradication of these microorganisms is not required. It is only important to cure the disease: urethritis, bacterial vaginosis, PID. In most cases, treatment of the sexual partner is not required.
Forecast. Prevention
Limiting the number of sexual partners, the use of barrier methods of contraception reduce the colonization of ureaplasmas. In cases where there is already a carriage of ureaplasmas, a preventive examination and consultation with specialized specialists is necessary before:
Bibliography
- Shepard MC. The recovery of pleuropneumonia-like organisms from Negro men with and without nongonococcal urethritis. Am J Syph Gonorrhea Vener Dis. 1954 Mar;38(2):113-24
- Waites K. et al, Mycoplasmas and ureaplasmas as neonatal pathogens. Clinical microbiol review, Oct 2005, 757-789
- Zhou YH, Ma HX, Shi XX et al. Ureaplasma spp. in male infertility and its relationship with semen quality and seminal plasma components. J Microbiol Immunol Infect. 2017 Jun 22
- Leli C, Mencacci A, Latino MA et al. Prevalence of cervical colonization by Ureaplasma parvum, Ureaplasma urealyticum, Mycoplasma hominis and Mycoplasma genitalium in childbearing age women by a commercially available multiplex real-time PCR: An Italian observational multicentre study. J Microbiol Immunol Infect. 2017 Jun 28
The causative agent of various diseases of the genitourinary organs is Ureaplasma Species. This is a collective concept that combines Urealyticum and Parvum ureaplasmas. These microorganisms lead to the development of urethritis, cystitis, vaginitis, prostatitis and other pathologies.
Ureaplasmas in the human body
Ureaplasma spices are opportunistic microbes that are found in the genitourinary tract. With normal immunity, they do not cause inflammation. The disease develops when the number of microbes increases sharply. When bacteria are detected in an amount of 10,000 CFU / ml, we are talking about a ureaplasma infection. Such pain needs medical treatment. Ureaplasmosis is diagnosed in men and women. Adolescents and people of working age are more often ill.
Ureaplasmosis is included in the list of sexually transmitted infections, but is not a sexually transmitted disease. This method of transmission of the pathogen determines the great social significance of this issue, since a sick person is a danger to his sexual partners. Ureaplasma spices is often isolated in biological material along with other microbes (gonococci, chlamydia, Trichomonas, pale treponema).

What is ureaplasma spices
Ureaplasma spp are microorganisms that are intermediate between viruses and bacteria. They have the following features:
In most cases, these microbes are isolated from patients aged 15–30 years. The reason - the maximum sexual activity. Most often, ureaplasmas cause inflammation of the mucous membrane of the urethra. If untimely treatment, microbes spread further, affecting the vagina, cervix, bladder, testicles, uterine appendages, seminal ducts and prostate gland.
How infection occurs
Ureaplasma SPP in women and men is often detected by chance during laboratory tests. Infection can occur long before the first symptoms appear. The main route of penetration of microbes is sexual. The danger is represented by unprotected contacts (vaginal, oral, anal). protects against infection.
 Contact-household transmission of microbes is less common. It is possible if a person uses someone else's underwear or washcloths. The probability of infection is very low, but it cannot be ruled out. An intrauterine mechanism for the penetration of microbes is possible when they enter the amniotic fluid and lead to infection of the child.
Contact-household transmission of microbes is less common. It is possible if a person uses someone else's underwear or washcloths. The probability of infection is very low, but it cannot be ruled out. An intrauterine mechanism for the penetration of microbes is possible when they enter the amniotic fluid and lead to infection of the child.
Risk factors for the development of ureaplasmosis are:
- earlier onset of sexual activity;
- unprotected sexual contacts;
- promiscuous sex life;
- homosexual relationships;
- young age;
- addiction to alcohol;
- antisocial lifestyle;
- addiction.
Symptoms can be triggered by stress, overwork, surgery, injury, severe chronic illness, immunosuppressive drugs, radiation or chemotherapy, lack of vitamins in the body, poor diet, diabetes, and acquired immunodeficiency syndrome.

Why are microorganisms dangerous?
These microorganisms cause ureaplasmosis. It occurs in acute or chronic form. With monoinfection, symptoms are often absent. A vivid clinical picture is characteristic of ureaplasmosis in combination with chlamydia or other STIs. The favorite localization of microbes is the urethra.
urethritis develops. In men, it is more difficult, since their channel is longer and narrower. With urethritis, burning and cutting (pain) are observed. They appear at the beginning of micturition, as a result of which the excretion of urine is difficult. On examination, reddening of the mucosa in the area of the external opening can be detected.
Other symptoms include . In men, they are cloudy and are observed mainly in the morning. Allocations are scarce. In women, they may be bloody. This is observed after sexual intercourse. The spread of ureaplasmas leads to damage to the testicles. This manifests itself in pain and discomfort. There may be pain on palpation.

The appearance of pain, dysuric phenomena and sexual dysfunction are characteristic signs. Pain occurs at the beginning and end of micturitions. It radiates to the sacrum and genitals. Urination becomes frequent. In sick men, sexual desire decreases and erection is difficult.
Discomfort occurs during intercourse. Ejaculation is difficult or occurs early. In women, ureaplasmas cause the development of cervicitis and vaginitis. There is pain in the lower abdomen. Complicated ureaplasmosis leads to the development of endometritis and adnexitis (salpingoophoritis). This is fraught with the development of infertility. In men, ureaplasmas cause orchitis, vesiculitis, and epididymitis. Testicles, appendages and seminal vesicles are affected.
How to identify pathology
 Before treating patients, the diagnosis should be clarified. To do this, you will need to identify the causative agent of the infection. The following research will be required:
Before treating patients, the diagnosis should be clarified. To do this, you will need to identify the causative agent of the infection. The following research will be required:
- linked immunosorbent assay;
- immunofluorescence reaction;
- cultural research;
- polymerase chain reaction.
All diagnostic methods are divided into serological, cultural and genetic. If ureaplasmosis is suspected, they are determined. The material for research is blood. The sowing of the epithelium of the mucosa taken during the smear is very informative. After isolation of colonies of microbes, their sensitivity to antibiotics is assessed. A swab in men is taken from the urethra, and in women - from the vagina, urethra and cervix.
Fighting methods
It is necessary to know not only what it is, but also how to cure the sick. With the release of a large number of microbes, systemic antibiotics are prescribed. They are used in the form of tablets and capsules. Macrolides and fluoroquinolones show the greatest activity against ureaplasma spices.

These include Ecomed, Forte, Suprax, Sumatrolid Solution and Cifran. In the case of a mixed infection, 5-nitroimidazole derivatives and tetracyclines are prescribed.
An important aspect of therapy is the stimulation of immunity. It is necessary for people with frequent relapses of ureaplasmosis.
Medicines such as Immunomax, Amiksin, Likopid and Immunal are used. Antifungal drugs are often included in the treatment regimen. They allow you to prevent fungal diseases that often accompany ureaplasmosis. administration of immunoglobulins is possible. With ureaplasma SPP, patients should adhere to the following rules:

How to prevent disease
It is not difficult to prevent the penetration of ureaplasmas into the body. To do this, you will need to do the following:
- have sex only with reliable partners;
- use a condom;
- in case of accidental contacts, treat the genitals with an antiseptic;
- lead a healthy lifestyle;
- do not use alcohol and drugs;
- observe simple rules of intimate hygiene.
It is necessary to maintain the immune status at the proper level. This is achieved through healthy sleep, taking vitamins, a variety of diets, frequent walks in the fresh air, hardening and playing sports. It is recommended to periodically take tests for STI pathogens. To prevent complications with already developed ureaplasmosis, you need to follow the medical instructions for taking medications. Infections can lead to serious consequences. If left untreated, there is a possibility of sexual dysfunction and infertility.
Ureaplasma SPP what is it and what you need to know to quickly get rid of the problem? Ureaplasma spices is a type of tiny bacteria that lives on the mucous membranes of the human genitourinary organs. These bacteria are opportunistic pathogens. They have the ability to cause diseases, but at the same time they can be found in perfectly healthy people.
Bacteria are small and lack a rigid cell wall, which is why they are called defective bacteria, but due to this property they can penetrate the smallest pores and quickly adapt to different types of antibiotics. Another important distinguishing property is the ability to hydrolyze urea to ammonia, which is called ureolysis.
Ureaplasma Species do not have DNA and are close in size to viruses. According to their characteristics, they are, as it were, a transitional link from viruses to bacteria.
Methods of infection
The source of infection with ureaplasmosis is a sick person. Ureaplasmosis is very widespread and is one of the most common infections transmitted through sexual contact. Also, the infection can be transmitted from mother to child during childbirth. More often, the bacterium is found on the genitals and in the nasopharynx of the child.
During childbirth, infection occurs during the passage of the fetus through the birth canal, and it threatens the development of acute pneumonia, bronchopulmonary dysplasia, even possible blood poisoning and inflammation of the meninges. The occurrence of cerebral palsy and the risk of developing a psychomotor index were observed. Untreated ureaplasmosis can provoke premature birth and lung damage in a newborn baby.

During pregnancy, infection is unlikely, since the fetus is reliably protected by the placenta. If ureaplasmosis is initially detected during pregnancy, then this is not a prerequisite for its termination. With adequate and timely treatment, the child is born completely healthy.
It has a chance of contracting ureaplasmosis during organ transplantation - this is a very rare, but still occurring route of infection.
The main causes of infection are the following factors:
- Beginning sexual activity at an early age.
- A large number of sexual partners (even when using barrier contraceptives).
- Urological, infectious and venereal diseases.
To provoke the activation of the reproduction of the bacteria Ureaplasma SPP can:
- The use of antibiotics.
- The use of hormonal drugs.
- Frequent stressful situations, deterioration in the quality of life.
In the study of the bacterium Ureaplasma SPP was detected in the vagina of healthy women in 60%, newborn girls in 30% of the subjects. Men are found much less frequently. They are temporary carriers of bacteria. In addition, this type of bacteria causes a lot of controversy about its harmfulness.
Ureaplasmas cannot be infected in pools, in public places of use.
Symptoms of ureaplasmosis
Ureaplasma can occur in acute and chronic form in any part of the genitourinary system. The most striking manifestation in acute form.

According to studies, it was found that the incubation period of ureaplasmosis lasts up to several months, depending on the state of the body of the infected person. And this fact complicates the correct diagnosis.
Ureaplasma Species, once in the genitourinary tract, may not show any symptoms for a very long time, and this sometimes lasts for several years. It all depends on physiological barriers. The main factor in protection against the manifestation of symptoms is a healthy microflora. When the balance is disturbed in it, the ureaplasma is activated and begins to multiply intensively. Bacteria begin their destructive activity. In this case, ureaplasmosis is diagnosed, although the disease does not show pronounced symptoms that bring concern to the sick.
Women may find a clear discharge from the vagina, a burning sensation when urinating. In the case of a weakened immune system, the infection can move further along the genitals, causing inflammation of the uterus or appendages (endometritis).
In men, the symptoms have similar signs: transparent and insignificant discharge from the urethra appears, soreness and burning sensation during urination. With the development of the disease, it can cause inflammation of the urethra, testicles and their appendages, bladder and prostate gland.

Sometimes, with a weak manifestation, Ureaplasma SPP can pass on its own, but this does not guarantee its cure. The bacterium Ureaplasma Species continues to be in the human body until the next failure in the immune system.
If ureaplasmosis becomes chronic, then it can provoke the formation of an adhesive process. For women, this threatens with narrowing of the fallopian tubes, and for men, the vas deferens.
Diagnostics
The most informative method is the polymerase chain reaction (PCR). To detect the infection, the patient's biological fluid is taken and the presence of the pathogen's DNA is determined. To detect bacteria, it is necessary to take the following tests: a swab from the urethra or vagina, urine, ejaculate in men.
An additional bacteriological examination is prescribed. It makes it possible to find out the type of pathogen and the antibacterial substance to which it has sensitivity.
Enzyme-linked immunosorbent assay (ELISA) provides information on the form of the course of the disease (acute and chronic). This method is used in rare cases, due to low accuracy.

The exact result of the analysis can be affected by violation of the rules for storing the material, its contamination and improper collection. The number of cells when taking biomaterial should not be less than 500.
Treatment Methods
Often people can live with these infections and be unaware of the existence of Ureaplasma Species. Depending on how the pathogen develops in the human body, appropriate treatment is prescribed.
The main treatment is the use of antibiotics:
- macrolides. This is Azithromycin or Sumamed.
- Fluoroquinolones. This group of drugs is characterized by a longer period of treatment, but the effectiveness is not worse than with macrolides. Usually, patients are cured of Ureplasma SPP bacteria with Suprax, Cifran or Avelox.
- Tetracyclines. In this disease, they are used only in case of ineffectiveness of treatment with the above drugs. The drugs of this group are characterized by an ineffective effect on the causative agent of the disease. Doxycillin or Unidox is prescribed.
Immunostimulants are prescribed to strengthen the immune system.
So do not underestimate the consequences of this disease, which means that the Ureaplasma Species bacteria in the body must be disposed of.
 Does ureaplasma pass by itself (can it pass on its own)?
Does ureaplasma pass by itself (can it pass on its own)? PCR analysis to detect chlamydia Chlamydia PCR how to do
PCR analysis to detect chlamydia Chlamydia PCR how to do COCs with different daily dosages: how to choose, an overview of the best drugs
COCs with different daily dosages: how to choose, an overview of the best drugs Ureaplasma parvum: characteristics, tests, symptoms in women and men, what is dangerous, whether it is necessary to treat
Ureaplasma parvum: characteristics, tests, symptoms in women and men, what is dangerous, whether it is necessary to treat Basic technologies for obtaining nanomaterials
Basic technologies for obtaining nanomaterials How to tell the time in English?
How to tell the time in English?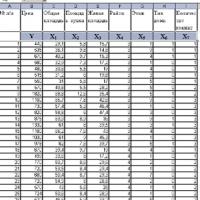 Introduction to Multivariate Statistical Analysis
Introduction to Multivariate Statistical Analysis