Ureaplasma 10 4. Ureaplasma parvum: characteristics, tests, symptoms in women and men, what is dangerous, whether it is necessary to treat. Ureaplasma - what is it
Ureaplasma is a microorganism that causes the development of a urogenital infection - ureaplasmosis. Infection in men most often occurs through sexual contact. Infection can be diagnosed using bacteriological culture, PCR studies, PIF and ELISA.
Ureaplasma 10 grade 4 indicates the development of an acute inflammatory process in the genitourinary system and requires antibiotic therapy. The choice of drug, dosage and duration of treatment depends on the severity of the disease and the age of the patient and is prescribed by the doctor on an individual basis.
What is ureaplasma?
Ureaplasma are small pathogenic microorganisms with a diameter of about 0.3 microns. They can cause a number of inflammatory pathologies of the genitourinary system, but in some cases they are also detected in healthy people. They have a negative impact on the body, starting to multiply actively, which occurs with a decrease in immunity.
The most dangerous are the following types of ureaplasma -. For similar characteristics they are combined into a group. According to statistics, parvum is much more common than urealiticum, but these bacteria affect the human body in the same way.
The main mode of transmission of ureaplasma is unprotected intercourse. This bacterium is able to exist in the body for a long time and does not manifest itself in any way. As the inflammatory process develops, it can affect the entire genitourinary system and cause a disease such as ureaplasmosis. The incubation period of this pathology is long - from 7 days to several months.
The main signs of infection are:
- transparent secretions of a mucous nature;
- frequent urge to urinate;
- itching and burning.
The first symptoms of the disease disappear on their own after a short time, which indicates the transition of ureaplasmosis into a chronic form. If left untreated, the inflammatory process begins to develop actively and can cause inflammation of the urethra, testicles, appendages, prostate and bladder. Most often, men go to the doctor with complaints not of ureaplasmosis, but of other diseases that this bacterium provokes.
In most people, ureaplasma does not manifest itself in any way, and they become carriers of this infection. They infect their sexual partners without even knowing it. Every year the number of people infected with latent sexual infections is only increasing.
Diagnostics
Before taking the tests for several days, it is necessary to refrain from sexual intercourse. On the day of biomaterial sampling, it is not necessary to wash the genitals. For 2-3 hours, a man should not urinate. It is not recommended to take any medications for about 7-10 days, and if there is a need for this, it is necessary to consult a specialist.
To detect ureaplasma, several types of studies are used, which are presented in the table:
Method | Description |
polymerase chain reaction | PCR is one of the most effective methods that allows you to identify the pathogen, even if it is present in the body in a small amount. The duration of the study is 1-3 days. When infected with ureaplasma, its quantity plays a significant role, therefore, if this bacterium is detected, an additional analysis will be required - bacteriological culture |
Bacteriological culture | This is the most common study that allows not only to identify pathogenic microorganisms, but also to determine their sensitivity to antibiotics. The biomaterial is placed in a special nutrient medium in which favorable conditions are created for the growth of ureaplasma. It takes about a week to complete this analysis. |
Direct immunofluorescence | The material is stained and then examined under a microscope. Pathogenic microorganisms become a certain color. Usually a couple of hours is enough for the analysis. |
Linked immunosorbent assay | The biomaterial is blood serum. This analysis reveals not an infection, but antibodies that are produced by the body during infection. With a positive result, PCR diagnostics or bacteriological culture are additionally performed, since the presence or absence of titers to ureaplasma does not allow an accurate diagnosis |
The appropriate research method is determined by the attending physician. To take the material, a special probe is inserted into the urethra, after which several translational movements are made to help scrape off particles of the mucosa. This is a necessary procedure, since ureaplasma does not multiply on the surface of the mucous membranes, but inside the cells.

Deciphering the results
The formulation of the result obtained depends on the choice of analysis. With the ELISA method (enzyme-linked immunosorbent assay), the number of antibodies present will be indicated and the result - positive or negative. Normally, antibodies to ureaplasma are absent. In the PCR study and bacteriological culture, the number of detected bacteria is indicated in the transcript.
Normally, in the biomaterial, the concentration of ureaplasma does not exceed 104 CFU / ml. With such an amount of it, the inflammatory process does not develop in the body, however, the man is a carrier of the infection and can infect sexual partners.
An indicator of 10 to the 3rd degree also indicates a carrier state. Even with such a low concentration of ureaplasma, an inflammatory process can develop, and in the event of a decrease in immunity, the bacterium begins to actively multiply, which leads to serious consequences. Even with indicators of 10 to the 2nd degree, a man can infect his sexual partners, despite the fact that he will not have any signs of the disease.
Ureaplasma 10 to the 5th degree is dangerous for the human body. At this concentration, ureaplasmosis begins to actively manifest itself and leads to acute inflammatory pathologies of the urethra. With indicators of 10 to the 6th degree or more, men usually already have urethritis, prostatitis, cystitis or pyelonephritis.

Treatment
In most cases, when the concentration of ureaplasma is less than 10 to the 4th degree, doctors do not prescribe treatment. But when planning the conception of a child, the treatment of all latent infections in both partners is mandatory, since bacteria can cause severe complications during pregnancy or provoke infertility.
- tetracyclines (doxycycline, Tygacil, tetracycline);
- macrolides (josamycin, clarithromycin, erythromycin);
- fluoroquinolones (ciprofloxacin, lomefloxacin, ofloxacin).

The duration of therapy, the choice of medications and their dosage depends on the severity of the disease. In chronic, it can last 3 weeks and includes 2 different antibiotics. If therapy does not have a positive result, the medications are replaced and a new treatment regimen is undergone.
Throughout the therapy, you need to give up sexual intercourse, drinking alcohol and smoking, fatty, salty and spicy foods. The sexual partner should also be treated, as re-infection is possible. Control tests are carried out after 2 weeks, and then after a month, and only in the case of two negative results can we talk about a complete cure.
Ureaplasma parvum (ureaplasma parvum) is the causative agent of genital infections in adults and children. These microbes are small and occupy an intermediate position between viral particles and bacteria.
Ureaplasma parvum freely persists on the mucous membranes of the genitourinary organs in healthy women, without causing the development of pathology and clinical symptoms. Under the influence of negative factors, the pathogenic activity of ureaplasmas increases, they begin to destroy mucosal cells and cause an inflammatory process.
Ureaplasma parvum is a conditionally pathogenic microorganism that is part of the vaginal biocenosis. The microbe has urease activity, a special life cycle and high contagiousness. When splitting urea, ammonia is formed, the excess of which can cause inflammation of the vagina, urethra, cervix, fallopian tubes.
Decreased immunity against the background of an infectious lesion of the genitourinary tract is the main reason., are able to lower the overall resistance of the body and local protection. These microbes and other pathogens of sexually transmitted infections are often found during the laboratory diagnosis of ureaplasmosis.
Ureaplasma parvum
This member of the mycoplasma family, together with ureaplasma urealiticum, was named "ureaplasma spp". Both of these microbes can cause similar diseases and provoke similar symptoms. Ureaplasma parvum is diagnosed predominantly in men, and ureaplasma urealiticum in women. Ureaplasma parvum is more pathogenic and leads to the development of a severe genitourinary infection. The disease proceeds for a long time with periods of exacerbation and remission.
Ways of spread of ureaplasma infection:

- Infection with ureaplasmosis occurs during intercourse with a sick person or a carrier. People who have promiscuous sex and neglect barrier contraception are at risk of getting sick with ureaplasmosis. In addition to traditional sexual intercourse, infection can occur during kissing, oral and anal caresses.
- Less common, but relevant is the vertical route of infection of the fetus and child during pregnancy and childbirth.
- The infection spreads through household contact in public places - transport, swimming pool, toilet.
- Infection can also occur during transplantation of donor organs.
Symptoms
Ureaplasma parvum is the cause of an acute or chronic inflammatory disease, the clinical symptoms of which are due to the location of the microbe.
Pathological signs that occur in sick women:

The disease caused by ureaplasma parvum is characterized by a long and often asymptomatic course. If treatment is not started in a timely manner, quite serious consequences can develop. In order not to miss the pathology, women are recommended to undergo regular examinations by a gynecologist and take appropriate tests. During pregnancy, physiological suppression of the immune system occurs. This is a normal reaction of the body, necessary for the development of the fetus, which contains the father's genetically alien antigens. That is why ureaplasmas in the body of pregnant women multiply rapidly and show their pathogenic properties. Ureaplasma parvum has a negative effect on the fetus, causing the development of dystrophy and infecting the fetal membranes. Newborns often develop meningitis and pneumonia. Ureaplasmosis can lead to miscarriages, malformations, premature birth. All pregnant women need to undergo a series of diagnostic tests to detect ureaplasma parvum.
Ureaplasmosis in the absence of adequate treatment can result in the development of severe complications in women - inflammation of the ovaries and uterus, the inability to conceive. In men, ureaplasma is fixed on spermatozoa and destroys them. The mobility of male germ cells gradually decreases, the general resistance of the organism is suppressed. At the same time, the quality of sperm deteriorates, its viscosity increases, and the number of spermatozoa in the seminal fluid decreases.
Diagnostics
To detect ureaplasma parvum, a number of diagnostic methods are used:
- Serodiagnostics- linked immunosorbent assay. The patient for research on an empty stomach take blood from a peripheral vein. In the blood, antibodies of various classes to Ureaplasma parvum are determined: IgG, IgA, IgM. A negative result of the analysis indicates the absence of infection in the body, and a positive result indicates that the patient is infected with ureaplasma.

- . PCR makes it possible to detect even one bacterial cell in the clinical material. This is a qualitative method for detecting characteristic RNA and DNA fragments inherent in ureaplasma parvum. Positive result - ureaplasma parvum (semicol.) DNA detected. A negative result is the absence of U. parvum DNA in the test sample. If ureaplasma DNA is found in the analysis, this means that there is a sexual infection ureaplasmosis.
- clinical material. Culture is one of the most effective diagnostic methods. First, biomaterial is taken. Usually examine the discharge of the vagina, urethra, blood, urine. The material is inoculated on special nutrient media, the cultures are incubated in a thermostat for several days, and the grown colonies are analyzed. Colonies of each type are counted. To isolate a pure culture, they are subcultured on storage media. After studying the tinctorial, cultural, biochemical and antigenic properties of the isolated microorganism, its sensitivity to antibiotics is determined. A diagnostically significant number of microbes is more than 10 to the 4th degree CFU / ml. If ureaplasma parvum is found in high concentration, treatment should be started immediately.

If the infection is not clinically manifested, and laboratory tests do not show a diagnostically significant titer of the pathogen, antibiotic therapy is not carried out, but the immune system is strengthened. Material for research from the cervical canal or urethra must be collected in the morning on an empty stomach with a special brush.
Women are subject to examination in order to identify ureaplasma pavrum:
- Suffering from chronic inflammatory diseases of the genitourinary system,
- who fail to conceive within a year of regular unprotected intercourse,
- who do not bear pregnancy,
- Who had a history of preterm birth before 34 weeks.
Treatment
Many people wonder if it is necessary to treat ureaplasma parvum? When the concentration of microbes in the test material exceeds 10 to the 4th degree CFU / ml and clinical signs appear, therapy should be started.
Treatment of ureaplasmosis caused by ureaplasma parvum involves the use of etiotropic agents - antibiotics, as well as immunostimulants, NSAIDs, vitamins, adaptogens.

Comprehensive treatment of pathology using all recommended groups of drugs will relieve symptoms and ensure a quick recovery. With repeated exacerbation of the pathology, other antibiotics are prescribed to patients. Ureaplasmas quickly adapt to antimicrobial agents. The treatment regimen must be adjusted each time during an exacerbation, introducing stronger drugs into it each time. Only following all the above recommendations can you completely recover from ureaplasmosis.
Venereal diseases are difficult to treat. It's better not to get infected. Prevention of ureaplasmosis consists in observing the rules of personal hygiene, using a condom, douching after intercourse with antiseptics, and having sex only with a regular partner.
Ureaplasma parvum is a microbe that is dangerous for a woman's body, causing various forms of inflammatory processes in the genitourinary system. Most pathologies caused by ureaplasma parvum are manifested by mild symptoms and are diagnosed late. That is why women should regularly visit a gynecologist and take all the necessary tests. Treatment of ureaplasmosis should be prescribed by a doctor, taking into account the individual characteristics of the patient.
Video: ureaplasma specialist
Ureaplasma in women refers to conditionally pathogenic microorganisms. Often the disease does not have characteristic manifestations, respectively, and mandatory antibacterial treatment is not carried out. Ureaplasma 10 to the 4th degree is the physiological concentration of bacteria in the body. This indicator indicates the possibility of an inflammatory process.
Ureaplasma, as a rule, affects the mucous membranes of the genitourinary system. To determine the presence of uraliticum and parvum, and to find out their titer, you need a smear with culture for microflora.

Before you take a smear, you need to stop taking medications that can affect the result of the study.
These bacteria became known to scientists in the middle of the 20th century. At that time, parvum and uraliticum were considered exclusively female bacteria, but in the 60s it became known that the stronger sex also had them.
In the process of various studies of the pathogenic microflora of the urethra and vagina, it became known that more than half of middle-aged people have these bacteria in their bodies. Thus, there was a need for diagnostic methods that could determine titers.
Important! Bubnovsky: "There is an effective treatment for ureaplasmosis! The disease will pass in a week if .."
New scientific work aimed to study the risk of developing the disease at different titers. Scientists have found that ureaplasma 4 CFU / tamp or more to the tenth degree is a certain milestone, overcoming which the bacterium becomes pathogenic and ureaplasmosis begins.
Before you take a smear, you need to stop taking medications that can affect the result of the study.
In the fairer sex, with indicators of 10 in the fourth degree, inflammation begins in the fallopian tubes. To determine ureaplasma urealyticum 10:4 CFU / tamp, you need to take a smear from the vagina or urethra in men, after which the bacterium is placed in a nutrient medium and titers are counted.
When results greater than 10:4 are obtained, culture should be tested for susceptibility to various antibiotics and therapy instituted. With indicators less than this value, the doctor can prescribe treatment only with obvious manifestations of inflammatory processes.
Ureaplasma with a titer of 10 4 CFU / tamp can be detected at an early stage of bearing a child. In this case, treatment, which could potentially harm, is postponed until the 20-22nd week of pregnancy in order to avoid pathology of fetal development. Some doctors prefer to start treatment immediately to exclude the possibility of progression of the pathology.
Normal performance
Quantitative detection of the norm of ureaplasma is optimally carried out using PCR and a bacterial smear. It is unreasonable to fully refer to a single source, since there is a high probability of error, which is associated with incorrect sampling of biomaterial. Also, preparation for analyzes may be insufficient or other factors will affect.
It is widely believed that it is necessary to ambiguously evaluate the criteria for the norm of ureaplasma, since it is not possible to accurately determine the number of bacteria in the human body.
According to the latest medical information, it is necessary to immediately undergo a therapeutic course for:
- the volume of ureaplasma significantly exceeding the norm;
- severe clinical manifestations;
- pregnancy and operations that are planned;
- associated infections.
If the analyzes show less than 10 per 4 copies in the sample, then in such an amount the bacterium has no clinical significance and antibacterial treatment is not required. Sometimes indicators are found in the 10th degree, which requires the appointment of additional tests.
Pathological concentration of ureaplasma
In women with similar indicators, inflammation in the fallopian tubes begins. A large number of pathogenic bacteria can lead to such ailments:
- endometritis,
- inflammation inside the fallopian tubes;
- cervical erosion;
- cystitis;
- decline in reproductive function.
Doctors are still arguing whether it is necessary to treat ureaplasmosis. Many studies suggest that therapy should be started already at an indicator of 8 10, especially during pregnancy.
Ureaplasma adversely affects the development of the fetus. If natural childbirth is carried out, the child becomes infected in 60% of cases.
A large number of doctors decide to bet on the immediate destruction of bacteria. This is justified by the fact that the probability of infection of the child during childbirth is high. If ureaplasma is 10 to 4 degrees or more, then mandatory therapy with the use of various medications is required.
Diagnostics
To identify the microorganism, a swab is taken from the vagina, cervix and urethra. These are the analyses:
- Real-time PCR: Expensive and not very common. Allows you to determine the amount and presence of the pathogen;
- cultural study is a sowing on nutrient media of microorganisms. A week later, colonies are counted, if there are more than 10 to the 4th degree CFU per ml, then a conclusion is made about the pathology;
- PCR allows you to determine the DNA of ureaplasma, does not show the volume;
- PIF and IFA.
Serological reactions are based on a blood test and the determination of antibodies to ureaplasma. Reactions determine the degree of immune response to pathology.
Treatment
The structure of therapy for the disease is practically the same in both sexes. Therapy is usually carried out with the help of tablets. The following medications may be prescribed:
- doxycycline;
- Josamycin;
- Azithromycin.
During treatment, you need to refrain from alcoholic beverages and sexual activity. Therapy of pregnant women is necessarily performed under the supervision of an obstetrician-gynecologist.
- Candles Genferon for women. They have anti-inflammatory and antibacterial effects, positively affecting the immune system;
- Candles Hexicon for men. They have an antiseptic effect, contribute to the active elimination of ureaplasma. Candles are used rectally.
In addition, the doctor may prescribe suppositories with an immunomodulatory effect. In addition, vitamin complexes are shown that increase the body's resistance.
After a certain time after the end of treatment, several tests are indicated to completely exclude the disease. If the tests are negative, the person is considered healthy.
Conclusion
It is important to remember that with any failure in the immune system or infection in the body, the pathological process develops rapidly. In order to prevent this from happening, you should consult a doctor in a timely manner, eat right, avoid severe stress and give up unprotected sex.
Ureaplasma spp. – a normal inhabitant of the human body, inhabiting the mucous membranes of the genitourinary organs and causing inflammation of the urogenital tract with a decrease in immunity. When the number of microorganisms in the discharge of the genital organs and urethra exceeds a certain threshold, the disease begins to manifest clinically: women have symptoms of vulvovaginitis, and men - or. After the detection of microbes, typing is carried out, during which the type of ureaplasmas and their number in the body are determined.
Ureaplasmosis is a ticking time bomb. This is an infectious disease transmitted mainly through sexual contact. Ureaplasmosis can be asymptomatic or manifest with pronounced clinical signs with each exacerbation. This is a rather unpleasant pathology, leading to a disorder of sexual function and infertility. Ureaplasma spp is considered a pathogenic and harmful to the body microbe, sexually transmitted.
In the absence of timely and adequate treatment, ureaplasmosis leads to the development of severe consequences: cystitis, arthritis, adhesions, infertility. The rate of development of these pathologies and complications has been growing rapidly in recent years. Ureaplasma spices often prevents couples from becoming parents.
Ureaplasma species
Ureaplasma spp is a gram-negative specific coccobacillus from the mycoplasma family, which is a transitional substance from a virus to a bacterium and does not have a cell membrane. Ureaplasma got its name due to its ability to hydrolyze urea.
 The favorite habitat of ureaplasma species is the urogenital area. In more rare cases, the microbe settles in the lung or kidney tissue. Ureaplasma spp is the common name for opportunistic microbes that have similar morphological and biochemical properties: ureaplasma urealiticum and ureaplasma parvum. The term "species" is used when PCR analysis reveals DNA structures characteristic of ureaplasma, without further research and determination of the type of ureaplasma.
The favorite habitat of ureaplasma species is the urogenital area. In more rare cases, the microbe settles in the lung or kidney tissue. Ureaplasma spp is the common name for opportunistic microbes that have similar morphological and biochemical properties: ureaplasma urealiticum and ureaplasma parvum. The term "species" is used when PCR analysis reveals DNA structures characteristic of ureaplasma, without further research and determination of the type of ureaplasma.
Ureaplasma species can persist for quite a long time on the mucous membrane of the genital organs and does not manifest itself in any way. Often, carriers of the infection find out about this quite by accident during a physical examination. People live quietly with ureaplasma spp all their lives, unaware of their presence.
Under the influence of adverse factors, the natural balance of microorganisms in the body is disturbed, ureaplasmas begin to multiply intensively and manifest their pathogenic properties, causing various ailments.
Factors contributing to the infection of ureaplasma species:
- Changes in the intestinal microflora,
- Decreased leukocytes in the blood
- Deterioration of the skin
- Immunodeficiencies,
- Chronic diseases of the urinary organs,
- Abuse of local antiseptics,
- Acid-base imbalance in the woman's vagina,
- bacterial,
- STI,
- Taking antibiotics and hormones
- Injuries of the genitourinary organs,
- frequent stress,
- hypothermia,
- Pregnancy, childbirth.
Ureaplasma spp is dangerous because it passes through micropores and is resistant to a number of antimicrobial drugs. The bacterium invades the genome of germ cells and disrupts their functions.
Epidemiology
The source and reservoir of infection are sick women and persistent carriers of ureaplasmas. Men are considered temporary carriers of the infection, capable of infecting women during intercourse.
Infection with ureaplasma spp. happens in several ways:
- Sexual - with oral-genital, vaginal and anal contact,
- Vertical - from a sick mother to a fetus during pregnancy and childbirth,
- Hematogenous - through an infected placenta and umbilical cord vessels,
- Transplantation - in organ transplantation,
- Hemotransfusion - with blood transfusion,
- Contact household - in extremely rare cases.
Sexual transmission of infection is most common. Infection usually occurs during unprotected intercourse. Since ureaplasmas are very small microorganisms, they can freely penetrate even through the pores of a condom. In people with strong immunity, pathology develops extremely rarely.
Ureaplasma spp is most often found in women who have several sexual partners, who are preparing to become a mother, undergoing hormone therapy, and in socially disadvantaged individuals.
Symptoms
In healthy people, ureaplasma spp does not manifest itself in any way. At the slightest malfunction in the body, immune defenses decrease, and clinical signs of ureaplasmosis appear.

In men, ureaplasmosis usually proceeds as urethritis, cystitis, pyelonephritis. Ureaplasma species nest in women in the vagina and in the uterine cavity. It causes cervical neoplasia, cervical insufficiency, urethral syndrome and urinary incontinence. Pre- and post-menstrual periods are the most suitable time for the appearance of clinical signs of the disease. The younger the woman, the more pronounced the symptoms of ureaplasmosis.
Clinical signs of diseases caused by ureaplasma species:
- Women have mild vaginal discharge without color and odor, sometimes with an admixture of blood; pain in the lower abdomen, aggravated during intercourse and immediately after it; itching and burning in the perineum; feeling of overflow of the bladder and other dysuric symptoms. Their libido decreases, and pregnancy does not occur for a long time. The mucous membrane of the cervix during examination is hyperemic and edematous.
- Men complain of cloudy, odorless discharge from the urethra that occurs in the morning; itching and burning in the perineum; lower abdominal pain; discomfort when urinating; soreness when touching the scrotum and head of the penis; decreased libido. In a man with ureaplasma, erectile dysfunction occurs, the consistency of sperm changes, sperm motility worsens, and their destruction occurs. Spermatogenic cells are deformed, sperm fluidity deteriorates.
These are symptoms of an acute form of pathology. In the absence of timely and adequate therapy, they gradually subside, the disease passes first into a subacute, and then into a chronic form. Patients have only a slight burning sensation and discomfort in the urethra and genitals. Patients often don't notice "mild" symptoms and trigger an infection. If the disease is not treated, adhesions may appear in the pelvic organs, narrowing the lumen of the fallopian tubes and blocking the seminal duct. Often the disease spreads up the urinary-genital tract.
Infected pregnant women often do not bear a child, they go into premature labor and are at increased risk of developing postpartum endometritis. If intrauterine infection of the fetus occurs, the newborn may develop pneumonia, malnutrition, and neuropathy.
Diagnostics

Diagnosis of ureaplasma infection in men begins with an external examination of the genital organs, palpation of the scrotum, rectal examination of the prostate. Then the patient is taken from the urethra, urine and seminal fluid and microscopic examination is carried out. Ultrasound of the prostate and scrotum allows you to confirm or refute the alleged diagnosis. In women, the vagina and cervix are examined, the ovaries are palpated, and a complete gynecological examination is performed. Microscopy of smears from the urethra, vagina and cervix, as well as ultrasound of the pelvic organs are additional diagnostic methods.
Laboratory diagnosis of diseases caused by ureaplasma species:

Treatment
During the treatment of ureaplasma infection, patients are advised to give up sexual activity, adhere to a certain diet, and not drink alcohol. Two weeks after the therapeutic course, control of cure is performed.

The course of treatment lasts an average of two months. The indicator of cure is a negative result of PCR diagnostics, indicating the complete destruction of microbes in the test sample. With a more severe damage to the body, treatment can be extended up to six months. A control analysis for the presence of ureaplasma spp is carried out after 2 weeks and a month after the end of treatment.
Ureaplasma species is the causative agent of urogenital infection, resistant to a wide range of antibiotics and does not cause persistent immunity after treatment, which is associated with frequent relapses of the disease.
Prevention
Preventive measures to prevent the development of ureaplasmosis:
- condom use,
- Treatment of the genital organs after sex with antiseptics,
- Hygiene of the genitals,
- Periodic testing for STIs,
- Regular visits to the gynecologist and urologist,
- Treatment of chronic diseases of the urogenital area,
- Maintaining a healthy lifestyle
- Strengthening immunity.
Ureaplasma species is present in the body of almost every person and quietly coexists with other bacteria without causing harm. But this does not mean that you can not pay attention to such “roommates”. The slightest excess of the allowable amount of these microbes often leads to the development of an individual reaction on the part of the body and causes various diseases.
Ureaplasma spices causes pathology in both sexual partners. Each of them should visit a doctor, undergo a diagnostic examination, based on the results of which intensive therapy will be prescribed.
Video: doctor about ureaplasma infection
Video: expert opinion on ureaplasma infection
 Does ureaplasma pass by itself (can it pass on its own)?
Does ureaplasma pass by itself (can it pass on its own)? PCR analysis to detect chlamydia Chlamydia PCR how to do
PCR analysis to detect chlamydia Chlamydia PCR how to do COCs with different daily dosages: how to choose, an overview of the best drugs
COCs with different daily dosages: how to choose, an overview of the best drugs Ureaplasma parvum: characteristics, tests, symptoms in women and men, what is dangerous, whether it is necessary to treat
Ureaplasma parvum: characteristics, tests, symptoms in women and men, what is dangerous, whether it is necessary to treat Basic technologies for obtaining nanomaterials
Basic technologies for obtaining nanomaterials How to tell the time in English?
How to tell the time in English?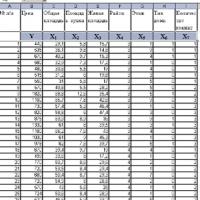 Introduction to Multivariate Statistical Analysis
Introduction to Multivariate Statistical Analysis