Choosing the best oral contraceptives. COCs with different daily dosages: how to choose, an overview of the best drugs
Each tablet combined oral contraceptives (COCs) contains estrogen and progestogen. Synthetic estrogen, ethinyl estradiol, is used as the estrogenic component of COCs, and various synthetic progestogens (synonymous with progestins) are used as progestogenic components.
Mechanism of contraceptive action of COC:
- suppression of ovulation;
- thickening of cervical mucus;
- change in the endometrium that prevents implantation.
The contraceptive action of COCs provides a progestogenic component. Ethinylestradiol as part of COCs supports endometrial proliferation and provides cycle control (no intermittent bleeding when taking COCs).
In addition, ethinyl estradiol is necessary to replace endogenous estradiol, since when taking COCs, there is no growth of the follicle and, therefore, estradiol is not produced in the ovaries.
The main clinical differences between modern COCs - individual tolerability, frequency of adverse reactions, features of the effect on metabolism, therapeutic effects, etc. - are due to the properties of their progestogens.
CLASSIFICATION AND PHARMACOLOGICAL EFFECTS OF COCs
Chemical synthetic progestogens - steroids; they are classified according to their origin.
Like natural progesterone, synthetic progestogens induce secretory transformation of the estrogen-stimulated (proliferative) endometrium. This effect is due to the interaction of synthetic progestogens with endometrial PR. In addition to affecting the endometrium, synthetic progestogens also act on other target organs of progesterone. The antiandrogenic and antimineralocorticoid effects of progestogens are favorable for oral contraception, and the androgenic effect of progestogens is undesirable.
The residual androgenic effect is undesirable, since it can be clinically manifested by the appearance of acne, seborrhea, changes in the lipid spectrum of blood serum, changes in carbohydrate tolerance and an increase in body weight due to anabolic effects.
According to the severity of androgenic properties, progestogens can be divided into the following groups:
- High androgenic progestogens (norethisterone, linestrenol, ethinodiol).
- Progestogens with moderate androgenic activity (norgestrel, levonorgestrel in high doses, 150-250 mcg / day).
- Progestogens with minimal androgenicity (levonorgestrel at a dose of not more than 125 mcg / day, including triphasic), ethinylestradiol + gestodene, desogestrel, norgestimate, medroxyprogesterone). The androgenic properties of these progestogens are found only in pharmacological tests, in most cases they have no clinical significance. WHO recommends the use of COCs with low-androgenic progestogens. In studies, it was found that desogestrel (active metabolite - 3ketodesogestrel, etonogestrel) has high progestogenic and low androgenic activity and the lowest affinity for SHBG, therefore, even at high concentrations, it does not displace androgens from its connection. These factors explain the high selectivity of desogestrel compared to other modern progestogens.
Cyproterone, dienogest and drospirenone, as well as chlormadinone, have an antiandrogenic effect.
Clinically, the antiandrogenic effect leads to a decrease in androgen-dependent symptoms - acne, seborrhea, hirsutism. Therefore, COCs with antiandrogenic progestogens are used not only for contraception, but also for the treatment of androgenization in women, for example, with PCOS, idiopathic androgenization, and some other conditions.
SIDE EFFECTS OF COMBINED ORAL CONTRACEPTIVES (COCs)
Side effects often occur in the first months of taking COCs (in 10-40% of women), in the subsequent time their frequency decreases to 5-10%. Side effects of COCs are usually divided into clinical and mechanism-dependent.
Excessive influence of estrogens:
- headache;
- increase in blood pressure;
- irritability;
- nausea, vomiting;
- dizziness;
- mammalgia;
- chloasma;
- worsening tolerance to contact lenses;
- weight gain.
Insufficient estrogenic effect:
- headache;
- depression;
- irritability;
- reduction in the size of the mammary glands;
- decreased libido;
- dryness of the vagina;
- intermenstrual bleeding at the beginning and middle of the cycle;
- scanty menses.
Excessive influence of progestogens:
- headache;
- depression;
- fatigue;
- acne;
- decreased libido;
- dryness of the vagina;
- deterioration of varicose veins;
- weight gain.
Insufficient progestogenic effect:
- heavy menstruation;
- intermenstrual bleeding in the second half of the cycle;
- delay in menstruation.
If side effects persist longer than 3-4 months after the start of treatment and / or increase, then the contraceptive drug should be changed or discontinued.
Serious complications when taking COCs are extremely rare. These include thrombosis and thromboembolism (deep vein thrombosis, pulmonary embolism). For women's health, the risk of these complications when taking COCs with a dose of ethinylestradiol 20-35 mcg / day is very small - lower than during pregnancy. Nevertheless, the presence of at least one risk factor for the development of thrombosis (smoking, diabetes mellitus, high degrees of obesity, arterial hypertension, etc.) is a relative contraindication to taking COCs. The combination of two or more of the above risk factors (for example, smoking over the age of 35) excludes the use of COCs altogether.
Thrombosis and thromboembolism, both when taking COCs and during pregnancy, can be manifestations of hidden genetic forms of thrombophilia (resistance to activated protein C, hyperhomocysteinemia, deficiency of antithrombin III, protein C, protein S; APS). In this regard, it should be emphasized that the routine determination of prothrombin in the blood does not give an idea of the hemostasis system and cannot be a criterion for prescribing or canceling COCs. When identifying latent forms of thrombophilia, a special study of hemostasis should be carried out.
CONTRAINDICATIONS TO THE USE OF COMBINED ORAL CONTRACEPTIVES
Absolute contraindications to taking COCs:
- deep vein thrombosis, pulmonary embolism (including history), high risk of thrombosis and thromboembolism (with extensive surgery associated with prolonged immobilization, with congenital thrombophilia with pathological levels of coagulation factors);
- ischemic heart disease, stroke (presence of a history of cerebrovascular crisis);
- arterial hypertension with systolic blood pressure of 160 mm Hg. and more and / or diastolic blood pressure of 100 mm Hg. and more and / or with the presence of angiopathy;
- complicated diseases of the valvular apparatus of the heart (hypertension of the pulmonary circulation, atrial fibrillation, history of septic endocarditis);
- a combination of several factors in the development of cardiovascular diseases (age over 35 years, smoking, diabetes, hypertension);
- liver diseases (acute viral hepatitis, chronic active hepatitis, liver cirrhosis, hepatocerebral dystrophy, liver tumor);
- migraine with focal neurological symptoms;
- diabetes mellitus with angiopathy and/or disease duration of more than 20 years;
- breast cancer, confirmed or suspected;
- smoking more than 15 cigarettes per day over the age of 35;
- lactation in the first 6 weeks after birth;
- pregnancy.
RESTORATION OF FERTILITY
After stopping the use of COCs, the normal functioning of the hypothalamus-pituitary-ovaries system is quickly restored. More than 85-90% of women are able to become pregnant within one year, which corresponds to the biological level of fertility. Taking COCs before conception does not adversely affect the fetus, the course and outcome of pregnancy. Accidental use of COCs in the early stages of pregnancy is not dangerous and does not serve as a basis for abortion, but at the first suspicion of pregnancy, a woman should immediately stop taking COCs.
Short-term use of COCs (within 3 months) causes an increase in the sensitivity of the receptors of the "hypothalamus-pituitary-ovaries" system, therefore, when COCs are canceled, tropic hormones are released and ovulation is stimulated.
This mechanism is called the "rebound effect", it is used in the treatment of certain forms of anovulation. In rare cases, after the abolition of COCs, amenorrhea can be observed. Amenorrhea may be the result of atrophic changes in the endometrium that develop when taking COCs. Menstruation appears when the functional layer of the endometrium is restored independently or under the influence of estrogen therapy. Approximately 2% of women, especially in the early and late periods of fertility, after stopping the use of COCs, amenorrhea can be observed lasting more than 6 months (hyperinhibition syndrome). The frequency and causes of amenorrhea, as well as the response to therapy in women using COCs, do not increase the risk, but may mask the development of amenorrhea with regular menstrual bleeding.
RULES FOR INDIVIDUAL SELECTION OF COMBINED ORAL CONTRACEPTIVES
COCs are selected for women strictly individually, taking into account the characteristics of the somatic and gynecological status, individual and family history data. The selection of COCs is carried out according to the following scheme:
- Targeted interview, assessment of somatic and gynecological status and determination of the acceptability category of the combined oral contraceptive method for this woman in accordance with the WHO acceptance criteria.
- The choice of a specific drug, taking into account its properties and, if necessary, therapeutic effects; counseling a woman about the COC method.
decision to change or cancel COCs.
- Dispensary observation of a woman during the entire period of COC use.
In accordance with the WHO conclusion, the following examination methods are not related to the assessment of the safety of the use of COCs:
- examination of the mammary glands;
- gynecological examination;
- examination for the presence of atypical cells;
- standard biochemical tests;
- tests for PID, AIDS.
The drug of first choice should be a monophasic COC with an estrogen content of not more than 35 mcg / day and a low-androgenic progestogen.
Three-phase COCs can be considered as reserve drugs when signs of estrogen deficiency appear against the background of monophasic contraception (poor cycle control, dryness of the vaginal mucosa, decreased libido). In addition, triphasic drugs are indicated for primary use in women with signs of estrogen deficiency.
When choosing a drug, one should take into account the characteristics of the patient's health status (Table 12-2).
Table 12-2. Choice of combined oral contraceptives
| Clinical situation | Recommendations |
| Acne and/or hirsutism, hyperandrogenism | Drugs with antiandrogenic progestogens |
| Menstrual disorders (dysmenorrhea, dysfunctional uterine bleeding, oligomenorrhea) | COCs with a pronounced progestogenic effect (Marvelon ©, Microgynon ©, Femoden ©, Jeanine ©). With a combination of dysfunctional uterine bleeding with recurrent endometrial hyperplastic processes, the duration of treatment should be at least 6 months. |
| endometriosis | Monophasic COCs with dienogest, levonorgestrel, desogestrel or gestodene, as well as progestin COCs, are indicated for long-term use. The use of COCs can help restore generative function |
| Diabetes mellitus without complications | Preparations with a minimum content of estrogen - 20 mcg / day |
| Primary or repeated administration of COCs to a smoking patient | When smoking under the age of 35 - COC with a minimum content of estrogen. Smoking patients older than 35 years COCs are contraindicated |
| Previous COC use was accompanied by weight gain, fluid retention in the body, mastodynia | Yarina© |
| Poor menstrual control has been observed with previous COC use (in cases where causes other than COC use are ruled out) | Monophasic or three-phase COCs (Three-Mercy ©) |
The first months after the start of taking COCs serve as a period of adaptation of the body to hormonal changes. At this time, intermenstrual spotting bleeding or, less often, breakthrough bleeding (in 30–80% of women), as well as other side effects associated with hormonal imbalance (in 10–40% of women), may occur.
If these adverse events do not go away within 3–4 months, this may be the basis for changing the contraceptive (after excluding other causes - organic diseases of the reproductive system, missing pills, drug interactions) (Table 12-3).
Table 12-3. Selection of COCs of the second line
| Problem | Tactics |
| Estrogen dependent side effects | Reducing the dose of ethinylestradiol Switching from 30 to 20 mcg / day of ethinylestradiol Switching from triphasic to monophasic COCs |
| Gestagen-dependent side effects | Dose reduction of progestogen Switching to a three-phase COC Switching to COC with another progestogen |
| Decreased libido | Switching to a three-phase COC- Switching from 20 to 30 mcg / day of ethinylestradiol |
| Depression | |
| Acne | Switching to COCs with antiandrogenic effect |
| Breast engorgement | Switching from a triphasic to a monophasic COC Switching to ethinylestradiol + drospirenone Switching from 30 to 20 mcg/day of ethinylestradiol |
| Vaginal dryness | Switching to a three-phase COC Switching to a COC with another progestogen |
| Pain in the calf muscles | Switching to 20 mcg/day of ethinyl estradiol |
| Scanty menstruation | Switching from monophasic to triphasic COCs Switching from 20 to 30 mcg/sutetinylestradiol |
| Abundant menstruation | Switching to a monophasic COC with levonorgestrel or desogestrel Switching to ethinylestradiol 20 mcg/day |
| Intermenstrual spotting at the beginning and middle of the cycle | Switching to a three-phase COC Switching from 20 to 30 mcg / day of ethinylestradiol |
| Intermenstrual spotting in the second half of the cycle | Switching to COCs with a higher dose of progestogen |
| Amenorrhea while taking COCs | Pregnancy must be ruled out Together with COC ethinylestradiol throughout the cycle Switching to COC with a lower dose of progestogen and a higher dose of estrogen, for example, triphasic |
The basic principles for monitoring women using COCs are as follows:
- in the annual gynecological examination, including colposcopy and cytological examination;
- in the examination of the mammary glands every six months (in women with a history of benign tumors of the mammary glands and / or breast cancer in the family), mammography once a year (in patients in perimenopause);
- in the regular measurement of blood pressure: with an increase in diastolic blood pressure up to 90 mm Hg. and more - stop taking COCs;
- in a special examination according to indications (with the development of side effects, the appearance of complaints).
In case of menstrual dysfunction - exclusion of pregnancy and transvaginal ultrasound scanning of the uterus and its appendages.
RULES FOR RECEPTION OF COMBINED ORAL CONTRACEPTIVES
All modern COCs are produced in "calendar" packages designed for one cycle of administration (21 tablets - one per day). There are also packs of 28 tablets, in which case the last 7 tablets do not contain hormones ("pacifiers"). In this case, the packs should be taken without interruption, which reduces the likelihood that the woman will forget to start taking the next pack on time.
Women with amenorrhea should start taking it at any time, provided that pregnancy has been reliably excluded. In the first 7 days, an additional method of contraception is required.
Women who are breastfeeding:
- earlier than 6 weeks after birth, COCs are not prescribed;
- in the period from 6 weeks to 6 months after childbirth, if the woman is breastfeeding, use COCs only if absolutely necessary (the method of choice is minipill);
- more than 6 months after birth, COCs are prescribed:
♦with amenorrhea - see the section "Women with amenorrhea";
♦with a restored menstrual cycle - see the section "Women with a regular menstrual cycle".
PROLONGED REGIME OF COMBINED ORAL CONTRACEPTIVES
Prolonged contraception provides for an increase in the duration of the cycle from 7 weeks to several months. For example, it may consist of taking 30 micrograms of ethinyl estradiol and 150 micrograms of desogestrel or any other COC continuously. There are several schemes of prolonged contraception. The short-term dosing scheme allows you to delay menstruation by 1-7 days, it is practiced before the upcoming surgery, vacation, honeymoon, business trip, etc. The long-term dosing regimen allows you to delay menstruation from 7 days to 3 months. As a rule, it is used for medical reasons for menstrual irregularities, endometriosis, MM, anemia, diabetes, etc.
Prolonged contraception can be used not only to delay menstruation, but also for therapeutic purposes. For example, after surgical treatment of endometriosis in a continuous mode for 3-6 months, which significantly reduces the symptoms of dysmenorrhea, dyspareunia, improves the quality of life of patients and their sexual satisfaction.
The appointment of prolonged contraception is also justified in the treatment of MM, since in this case the synthesis of estrogens by the ovaries is suppressed, the level of total and free androgens decreases, which, under the action of aromatase synthesized by the tissues of the myoma, can turn into estrogens. At the same time, women do not observe estrogen deficiency in the body due to its replenishment with ethinyl estradiol, which is part of the COC. Studies have shown that in PCOS, continuous use of Marvelon© for 3 cycles causes a more significant and persistent decrease in LH and testosterone, comparable to that with the use of GnRH agonists, and contributes to a much greater decrease in these indicators than when taken in a standard regimen.
In addition to the treatment of various gynecological diseases, the use of the method of prolonged contraception is possible in the treatment of dysfunctional uterine bleeding, hyperpolymenorrhea syndrome in perimenopause, as well as in order to relieve vasomotor and neuropsychiatric disorders of the climacteric syndrome. In addition, prolonged contraception enhances the oncoprotective effect of hormonal contraception and helps prevent bone loss in women of this age group.
The main problem of the prolonged regimen was the high frequency of "breakthrough" bleeding and spotting, which is observed during the first 2-3 months of admission. The data currently available indicate that the incidence of adverse reactions with extended cycle regimens is similar to those for conventional regimens.
RULES OF FORGOTTEN AND MISSED PILLS
- If 1 tablet is missed:
♦ delay in taking less than 12 hours - take the missed pill and continue taking the drug until the end of the cycle according to the previous scheme;
♦ being late for more than 12 hours - the same actions plus:
- if you miss a tablet in the 1st week, use a condom for the next 7 days;
- if you miss a pill on the 2nd week, there is no need for additional contraceptives;
- if you miss a tablet on the 3rd week, after finishing one package, start the next one without a break; there is no need for additional protective equipment. - If 2 or more tablets are missed, take 2 tablets per day until regular intake, plus use additional methods of contraception for 7 days. If bleeding occurs after the missed tablets, it is better to stop taking the tablets from the current package and start a new package after 7 days, counting from the start of the missed tablets.
RULES FOR PRESCRIBING COMBINED ORAL CONTRACEPTIVES
- Primary appointment - from the 1st day of the menstrual cycle. If the reception is started later (but no later than the 5th day of the cycle), then in the first 7 days it is necessary to use additional methods of contraception.
- Appointment after abortion - immediately after the abortion. Abortion in the I, II trimesters, as well as septic abortion are classified as category 1 conditions (there are no restrictions on the use of the method) for the appointment of COCs.
- Appointment after childbirth - in the absence of lactation - not earlier than the 21st day after childbirth (category 1). In the presence of lactation, do not prescribe COCs, use minipill no earlier than 6 weeks after birth (category 1).
- The transition from high-dose COCs (50 micrograms of ethinylestradiol) to low-dose (30 micrograms of ethinylestradiol or less) - without a 7-day break (so that the hypothalamic-pituitary system does not activate due to dose reduction).
- Switching from one low-dose COC to another - after the usual 7-day break.
- The transition from minipili to COC - on the first day of the next bleeding.
- Switching from an injectable to a COC is on the day of the next injection.
- Switching from a combined vaginal ring to a COC - on the day the ring was removed or on the day a new one was to be introduced. Additional contraception is not required.
Currently, oral contraceptives, the list of which is quite large, are used by women very widely. But when using hormonal contraceptive pills for women, one should be clearly aware of both the positive and negative aspects of using these drugs.
Given that the list of hormonal drugs currently offered is very large, women need to understand what classification of these drugs is used, what contraindications and side effects they have in order to take into account all the risks associated with their use. It is also necessary to take into account the positive aspects that such contraception provides for women.
Thus, every woman should be clearly aware that when interfering with the natural processes occurring in the body, there are consequences that are manifested differently for everyone.
Therefore, any contraceptives for girls and women should be selected by a gynecologist who can adequately assess all contraindications and side effects. hormonal drugs . It is up to the doctor to explain in detail what is oral contraceptives how to take modern oral contraceptives, as well as explain all their pros and cons.
On the Internet you can also find a lot of information, as well as photos and videos on this topic.
Groups of contraceptives, their action
Modern pharmacology offers a very extensive range of new generation contraception. It is the list of new generation hormonal contraceptives that is the most in demand and popular. But even with the ease of obtaining the necessary information in the modern world, not everyone knows how to choose the right drugs for protection, what side effects can be, how long the intake can last.
Wikipedia shows that hormonal contraceptive pills are divided into two large groups:
- (abbreviated COC);
COCs contain (those who are interested, ethinylestradiol - what it is, you should know that this substance is a synthetic analogue), as well as progestogen (gestodene, norgestrel, norethisterone, desogestrel, etc.). Depending on which hormones the drugs contain, three-phase, two-phase and monophasic contraceptives are distinguished.
The problem of protection from unwanted pregnancy is very relevant. According to statistics, more than half of all conceptions are unplanned. This situation can sometimes end in the birth of a healthy child, but more often followed by artificial termination of pregnancy or other undesirable outcomes. Much is decided by chance. However, in the modern world, relying on fate in the matter of procreation is not worth it. The pharmaceutical industry produces various types of contraceptives that have several mechanisms of action and a fairly high efficiency. The leading place belongs to hormonal agents.
Tablets, implants, injectables and transdermal releasing systems have the maximum ability to prevent ovulation, fertilization of a mature egg and its implantation. All this makes an unwanted pregnancy almost impossible. The most widespread are tableted hormonal contraceptives, popularly referred to as "contraceptive pills". The choice of this dosage form is associated with traditional preferences, and with wide availability, and ease of use.
Combined oral contraceptives
So beloved by gynecologists, combined oral contraceptives (COCs) are pills to prevent unwanted pregnancy, which include two active hormonal components (estrogens and gestagens). The introduction of contraceptive pills into practice in the 60s of the 20th century led to profound social changes in society. In fact, for the first time, a woman was able to have an active sexual life without the danger of unwanted pregnancy and plan the birth of her children. Historians credit the emergence of COCs as responsible for the sexual revolution in the Western world. What are these tablets? How much have they changed over the past decades?
The mechanism of action of contraceptive pills
The mechanism of action of COCs is realized at the level of cellular receptors. Estrogens and gestagens of tablets block receptors in the organs of the female reproductive system.
As a result of this, firstly, inhibition of ovulation occurs. The growth and maturation of eggs is suppressed due to a decrease in the concentration and normal rhythm of secretion of pituitary hormones - luteinizing and follicle-stimulating.
Birth control pills also affect the inner lining of the uterus. There is a "glandular regression" in it. This means that the endometrium will practically atrophy, and if suddenly the egg is still able to mature and be fertilized, it will be impossible for it to implant in the uterus.
Another important effect of COCs is a change in the structure of mucus in the cervix. The viscosity of this secret increases and the entrance to the uterine cavity for spermatozoa is actually blocked.
Fourthly, birth control pills also affect the adnexa of the uterus - the fallopian tubes. Their contractile activity falls, which means that the movement of the egg along them becomes almost impossible.
The contraceptive effect of COCs is more associated with the inhibition of ovulation (egg maturation). Pills create an artificial cycle in a woman's body, suppressing the normal menstrual cycle. The physiology of the reproductive system is based on the principle of "feedback". That is, the pituitary gland produces tropic hormones (in this case, follicle-stimulating) in response to a decrease in the level of target organ hormones (in this case, estrogens and progestogens in the ovaries). If a sufficiently large amount of estrogens and progestogens enters the woman's body from the outside, then tropic hormones in the pituitary gland cease to be produced. This leads to a lack of growth and development of eggs in the ovaries.
The level of hormones in the blood when taking COCs is quite individual. Specific figures depend on the weight of the woman, the percentage of adipose tissue in her body, the level of sex-binding globulin in the blood. Studies of progesterone and estrogen are considered inappropriate while taking pills. Theoretically, the concentration of estrogens and gestagens after taking high-dose COCs is comparable to the hormonal background of pregnancy. With low- and microdosing drugs, these levels are lower than during pregnancy, but higher than during a normal menstrual cycle.
Types of combined oral contraceptives
COCs are divided into groups depending on the concentration of hormones and division into phases.
As an estrogen tablets usually contain estradiol. Ethinyl estradiol is currently being used. With regard to the concentration of estrogens, over the five decades of COC use, it has progressively decreased. In 1960, estradiol in one tablet was 150 micrograms. Currently, its dose is much lower and can be as low as 15-20 micrograms. Tablets are divided into high-dose (more than 35 mcg), low-dose (30-35 mcg), microdosed (less than 30 mcg).
The negative effects of large doses of estrogens (more than 50 micrograms per day) made the use of first-generation COCs rather unsafe in a number of women. The most serious complications are violations in the blood coagulation system - thrombosis and embolism. Modern low-dose and micro-dose birth control pills are much less likely to cause such complications. However, disturbances in the hemostasis system are a contraindication to prescribing even modern COCs.
As gestagens synthetic derivatives of norsteroids and progesterone are used. The dose of gestagens also gradually decreased from the 60s to the present (from 9.85 to 0.15-0.075 mg).
The first generation of norsteroid progestogens: noretinodrel, linesterenol, norgesterel, etinodiol diacetate, norgestimate, norgestrel.
First generation progesterone: medroxyprogesterone acetate, cyproterone acetate, chlormadinone acetate. The improvement of this component of COCs followed the path of reducing undesirable glucocorticoid and androgenic effects.
Modern derivatives of norsteroils are levonorgestrel, desogestrel, gestodene, norgestimate. The new progestogen drospirenone is a derivative of spirolactone.
Old gestagens increase the atherogenic properties of the blood, can contribute to the development of arterial hypertension, reduced glucose tolerance, fluid retention, the appearance of seborrhea and hirsutism. Modern gestagens do not affect the metabolism (lipids, glucose).
Cyproterone acetate and drospirenone have an antiandrogenic effect. They can be used to treat hirsutism, acne, seborrhea, hair loss. COCs with these components - Diane-35 (35 μg ethinylestradiol and 2 mg cyproterone acetate) and Yarin (30 μg ethinylestradiol and 3 mg drospirenone), Jess (20 μg ethinylestradiol and 3 mg drospirenone). Other modern gestagens in combination with estrogens also have a positive effect on the condition of a woman's skin and hair. These drugs are Femoden, Marvelon, Regulon, Silest, Jeanine, Mercilon, Logest, Novinet, Mirelle, Lindinet, Tri-Merci.
Drospirenone helps to reduce fluid retention in the body. Yarina and Jess are successfully used to treat premenstrual syndrome, as it is mainly caused by latent tissue swelling.
COC tablets are divided into three types: one-, two-, three-phase. This classification is based on the concentration of substances in tablets.
V single phase birth control pills the dose of the components is constant. In biphasic and triphasic COCs, an attempt was made to imitate the normal menstrual cycle of a woman - its follicular and luteal phases. In the natural cycle in women after ovulation, the level of progestogens in the blood increases sharply.
V biphasic COCs the first 11 tablets contain estrogens and gestagens in a ratio of 1:1, the next 10 - 1:2.5. An example is Anteovin (ethinylestradiol 50mcg and levonorgestrel 0.05mg-0.125mg). The high dose of estrogen makes these drugs unattractive.
Triphasic birth control pills are used more often. Phases may have a different number of tablets. In Tri-Merci, each phase is 7 days (ethinylestradiol 35-30-30 mcg and desogestrel 0.05-0.1-0.15 mg). Examples of three-phase COCs are also Triquilar, Tri-regol, Triziston.
The most common COCs are single-phase. They do not mimic the natural menstrual cycle, but they consistently suppress ovulation with relatively little estrogen demand.
Examples of high-dose single-phase COCs– Ovidon, Non-Ovlon; low-dose- Rigevidon, Microgynon, Minisiston, Femoden, Marvelon, Regulon, Silest, Diane-35, Zhanin, Yarina; microdosed- Mercilon, Logest, Novinet, Mirelle, Lindinet, Jess.
Choice of birth control pills
Which COCs will be prescribed, the doctor decides. Choosing pills on your own is dangerous to health. Side effects of drugs and contraindications to their use can only be assessed by a gynecologist during an internal consultation and after an appropriate examination.
Today, modern preparations are considered optimal - low- and micro-dosed, containing 20-30 micrograms of ethinyl estradiol and modern gestagens.
Low-dose triphasic COCs (Tri-Merci) are recommended for young women without children. Teenage girls with acne and seborrhea can be prescribed this particular drug - its effect on the pituitary gland and the entire functional activity of the reproductive system is the least, which is especially important at a young age and before the first birth. It is also acceptable to use microdose COCs in girls before childbirth (ethinyl estradiol 15-20 mcg).
For women who have given birth, single-phase COCs can be recommended. They are chosen depending on the clinical situation.
With the phenomena of increasing androgens (acne, seborrhea, hirsutism), Diane-35, Yarina, Jess are prescribed.
With the phenomena of premenstrual syndrome, COCs with drospirenone are chosen (Yarina, Jess).
In diabetes mellitus, only low- and micro-dosed COCs can be used. Preference should be given to single-phase microdosed tablets (Mersilon, Logest, Novinet, Mirelle, Lindinet, Jess).
In the presence of intermenstrual bleeding (ovulatory) discharge, single-phase contraceptives are chosen - the first 2-3 cycles are high-dose (Non-Ovlon, etc.), and then low-dose (Regulon, Rigividon, etc.)
With functional ovarian cysts, microdose contraceptive pills (Logest, Lindinet, Jess) are selected for 21 days with a 7-day break for a period of at least 6 months.
With erosion of the cervix, a thorough examination of the defect on the mucosa is carried out. Hormone therapy is carried out when an ectopic columnar epithelium of a dyshormonal nature is detected using micro- and low-dose single-dose COCs. Some gynecologists prefer three-phase preparations.
Mastopathy in a woman under 45 before the first birth and lactation should be a reason to refrain from long-term (more than 5 years) taking COCs. Modern low- and microdose tablets are considered a prophylactic for the prevention of fibrocystic mastopathy.
Before the doctor selects a COC, it is necessary to undergo an appropriate examination. Most likely, colposcopy and cytological examination of the endocervix, cervix, ultrasound examination of the pelvic organs, and mammary glands will be required. Women after 35 years of age are additionally prescribed a blood test for lipid spectrum (cholesterol and its fractions, triglycerides), analysis of the hemostasis system (prothrombin, fibrinogen, plasmin, antithrombin III), glycosylated hemoglobin or oral glucose tolerance test, ultrasound examination of the liver, gallbladder. The examination needs to be repeated annually.
Contraindications to taking birth control pills
COCs are absolutely contraindicated for women with thrombophlebitis, thromboembolism, vascular diseases of the brain, heart attack, stroke, previously and at the present time. Severe diseases of the liver, kidneys with impaired function and severe cardiovascular insufficiency are also considered an absolute contraindication to the use of COCs. It is impossible for contraceptive pills and nursing mothers.
The use of COCs is undesirable for migraines, epilepsy, stomach ulcers, hypertension, complications during a previous pregnancy in the form of diabetes or jaundice.
Sometimes there may be situations when COCs need to be canceled urgently. These include: high blood pressure, sudden visual disturbances, severe weight gain, planned surgery, a long period without movement (for example, due to injury).
Side effects of combined oral contraceptives
Microdosed COCs rarely lead to fatigue, weight gain, increased appetite, and decreased libido. With high-dose tablets, these phenomena are quite pronounced. Nausea, soreness of the mammary glands, intermenstrual bleeding can be within 2-3 months from the start of taking the pills and this is NOT an indication for drug withdrawal.
Switching to other COCs should be recommended by a doctor. Breakthrough bleeding causes a switch to higher-dose birth control pills. The appearance of symptoms of fluid retention in the body makes one prefer COCs with drospirenone as a progestogen (Jess, Yarina).
In women with an initially irregular cycle, long-term (more than 2-3 years) use of COCs can lead to the development of amenorrhea. Menstrual-like bleeding disappears and after the abolition of COCs, the cycle does not recover on its own. It is associated with ovarian hyperinhibition syndrome due to dysfunction of the pituitary gland. In this case, treatment is necessary.
Current data on the use of low- and microdosed COCs demonstrate their safety in relation to the development of oncology of the reproductive system. There is no definitive answer to the question of the effect of birth control pills on the risk of breast cancer. Most likely after 45 years, the risk of breast cancer when taking COCs is not higher than with other types of contraception.
When taking COCs, the incidence of endometrial cancer is reduced by 50%. The incidence of epithelial malignant ovarian tumors is reduced by at least 40% (up to 80% when taken for more than 5 years). In women with initially disturbed hormonal balance, the preventive role of COCs is higher.
How to take COC tablets?
A pack of tablets for a month contains 21 (24) active tablets, that is, COCs with hormones. Some of the drugs also include placebos - "empty pills" that do not contain hormones, but are included for ease of administration. Single-phase COCs (21 tablets) are taken from days 5 to 25 or from 1 to 21 days of the cycle. Multi-phase tablets must be taken from the 1st day of the cycle. Then they take a break of 7 days. If the COC contains a placebo, then the tablets are drunk without interruption.
Tablets are taken at the same time with a small amount of water. If the delay in taking the drug was less than 12 hours, the contraceptive effect is not reduced. The woman should take the missed pill as soon as possible and take the next one at the usual time.
If the delay in taking the next pill was more than 12 hours, contraceptive effectiveness may be reduced.
If a woman has had vomiting or diarrhea during the first 4 hours after taking the active tablets, absorption may not be complete and the woman should take additional contraceptive measures. As an additional measure, a barrier method - a condom - is usually recommended.
Other hormonal contraceptive pills
In addition to COCs, there are also single-component hormonal tablets. They contain only gestagen. Currently, the scope of these drugs is mainly the period of breastfeeding in women who are sexually active. Gestagens do not affect the quality and quantity of breast milk and do not have a negative effect on the baby. While estrogens have a pronounced effect on both lactation and the health of the child. Traditionally, "mini-drank" tablets are used. The problem with their use is the dependence on the time of admission - being late by 3 hours already increases the risk of pregnancy. Of the modern drugs, Desogestrel (75 mcg) is recommended. It can be taken without fear even 11-12 hours late.
Hormonal pills "after" (for postcoital contraception)
Emergency (postcoital) contraception is a method of preventing pregnancy after unprotected intercourse.
Emergency contraception is worse for a woman's health and less effective. The sooner action is taken, the greater the chance of avoiding an unwanted pregnancy. The proximity of ovulation, that is, the day of the cycle, also matters. On the day of ovulation, such contraception is less effective.
Postinor is used most often. It contains 0.75 mg of levonorgestrel. There are two tablets in the package. They must be taken sequentially with an interval of 12 hours on the first day after intercourse. Further, the efficiency drops.
High-dose COCs can be used as emergency contraception "after". Non-Ovlon (or another similar COC) is taken in the amount of 2 tablets immediately after sexual intercourse and 2 more tablets 12 hours later.
Another substance, the antiprogestogen mifepristone, is increasingly used as a means of emergency contraception. It is recommended 600 mg once within 72 hours after intercourse, or 200 mg on days 23-27 of the cycle, or: 25 mg 12 hours 2 times after intercourse. Now the drug at a dose of 10 mg has appeared on the market as a means of postcoital contraception. It has been proven to be highly effective with few side effects. It is possible to use 10 mg of the drug once within 120 hours after unprotected intercourse with a very high contraceptive effect. The advantage of the drug is its activity even in relation to the pregnancy that has already begun in the short term.
Endocrinologist Tsvetkova I.G.
Content
If a woman is sexually active, but does not feel ready for motherhood, she is faced with the question of which birth control pills are good, how to drink them, and what is the difference between hormonal and non-hormonal drugs. Is it possible to completely avoid the risk of getting pregnant if you use contraceptives regularly, and is there any chance of avoiding withdrawal syndrome?
What are birth control pills
Protection on the part of a man, if it is only a condom, does not give a 100% guarantee that the spermatozoa will still not penetrate the vagina and reach the developed eggs. Experts say that only good birth control pills help prevent pregnancy. They are divided into 2 groups: vaginal and oral. Main characteristics:
- Vaginal tablets have only a local effect, so they are used before sex. Their long-term use with any composition is not recommended. These pills cannot be classified as particularly reliable - they prevent pregnancy by only 70%. Pharmatex, Erotex, Gynecotex are the names of the most famous and working vaginal spermicides.
- Oral contraceptives (the preferred method of protection) have a different principle of action: they suppress ovulation with long-term use, the course is tied to a monthly cycle. Mostly in modern gynecology, combined oral contraceptives are used, based on a combination of the main female hormones: estrogen and progesterone. Among those especially recommended by gynecologists are Minisiston, Jess.
Monophasic
If the instruction suggests that you can drink the contents of the blister in any order, these are single-phase or monophasic COCs: all tablets will contain the same doses of active ingredients. From the standpoint of convenience, they are the best, according to women, and they are in the lead in the overall ranking of hormonal combined contraceptives. However, doctors argue that monophasic drugs are the least physiological, since it is natural for the body to change the hormonal background during the menstrual cycle.
Members of this group:
- Silest;
- Femodene;
- Mercilon.
Two-phase
If we look for a compromise between single-phase and three-phase contraceptive drugs, these will be two-phase: they suggest 2 types of tablets in a blister, differing in combinations of estrogen with progestin (the share of the latter is increased). They have side effects less often than monophasic ones, as they become closer to the natural processes in the female body. Their degree of protection is high, the doses of hormones are average, so it is easier to choose two-phase contraceptives for a sensitive organism than three-phase ones. Members of this group:
- Dimia;
- Nuvelle.
Triphasic drugs
The most natural for a girl's body are combined contraceptives, the dosage of active substances in which changes during the cycle. Triphasic drugs have a special regimen, according to which at each stage of the menstrual cycle, different doses of estrogen with progestin are supplied to the body, so there are fewer adverse reactions with such pills. If the specialist is able to choose the right birth control for you, protection against unwanted ovulation will be 100%.
Among the three-phase COCs, the following stand out:
- Triziston;
- Tri-merci.
Classification of COCs according to the content of active ingredients
When considering combined contraceptives, doctors recommend paying attention to the proportion of estradiol, since it is more responsible for ovulation and possible negative consequences from taking the drug. The amount of progestogen changes significantly only in two-phase COCs at the 1st and 2nd stages of the cycle, which almost does not play a role for the general classification.
Microdosed hormonal agents
In patients under 25 years of age, the use of combined contraceptives for a long time by gynecologists is not recommended due to the large number of adverse reactions that occur with the accumulation of synthetic hormones. Gynecologists recommend that girls pay attention to microdose contraceptives, where the amount of estrogen does not exceed 20 micrograms:
- Lindinet-20 - with long-term use (from 3 months) removes pain during the cycle, is often prescribed after scraping the epithelium for its growth.
- Zoeli is a combination of estrogen and nomegestrol, both components of natural origin, which distinguishes this medicine from other COCs.

Low dose birth control pills
Women who have already given birth, or those who, while taking microdose contraceptives, have experienced spotting bleeding (due to low estrogen), can try options with a higher dose of synthetic estradiol: this is 30 mcg. Most of the drugs whose names are heard through advertising are included in this group. The most effective:
- Tri-merci is a three-phase OK, created on the basis of estradiol with desogestrel, which normalizes hormonal levels well, but depresses libido. After cancellation, a strong hormonal failure is noticeable.
- Diane-35 - contains 35 mcg of estradiol combined with cyproterone, has a strong antiandrogenic effect, can be used to treat acne and hirsutism.
High-dose drugs
If the previous categories did not suit the woman, the doctor may consider the advisability of using hormonal drugs with 50 mcg of estradiol and above. You cannot buy such contraceptives without a specialist prescription: they greatly change the hormonal background, they are mainly used to treat diseases of the endocrine and reproductive systems. Often gynecologists prescribe:
- Triquilar - the reliability of this COC is high, the amount of estrogen reaches only 40 mcg, levonorgestrel - 25 mcg. Compared to other three-phase options, it is easier to tolerate.
- Triseston - the body must be absolutely healthy to receive this OK (especially relevant for the heart), smoking cannot be combined with it at all, but protection against pregnancy is up to 98%.
mini pili
Low-dose drugs of a non-combination type contain only a gestagen, the proportion of which ranges from 300-500 mcg. Mini-pills affect only the cervical mucus, thickening it, which prevents sperm from passing through it or implantation of the embryo. Their advantage is the ability to get by with minimal adverse reactions, permission to receive during lactation, but their effectiveness is not higher than 95%.
Most Popular:
- Microlute - each mini-pill contains 0.03 mg of progestogen, you need to drink 1 pc every day, according to a strict schedule (at the same hour). The sequence is maintained according to the scheme attached to the blister; the mini-pill is taken from the first day of the cycle.
- Charozetta - these contraceptives contain 0.075 mg of a progestogen, which increases their effectiveness if taken according to the instructions. These mini-pills do not affect hemostasis and metabolic processes, they have a small number of contraindications.

How to choose birth control pills
All types of drugs that prevent unwanted pregnancy are divided into 3 large categories, each of which works under certain conditions. Deciding which contraceptive pills are best to take should not only be based on ratings and reviews, but after clarifying the situation in which you find yourself. Medicines can be topical or oral, used before or after sexual intercourse.
Hormonal oral contraceptives
To influence the reproductive system of a woman, one cannot do without the use of hormones, and the most important here are estrogen and progestogen of synthetic origin. On their basis, several dozen modern contraceptives were created, divided into 3 groups:
- Based on estrogens - are used mainly as a medicine for deficiency of this hormone. They make sense in amenorrhea, during menopause. Ginodiol, Estrace - the most famous names of such drugs. The downside lies in the frequent intolerance of large doses of estrogen in women.
- With a high dose of gestagens (Lactinet, Exluton) - otherwise called mini-pills, they are considered good contraceptives for lactating women, but do not correct the menstrual cycle, do not suppress ovulation. After cancellation, the body recovers without obvious difficulties. The dosage of hormones is low.
- The combined type (Silhouette, Jess) involves a different ratio of estrogens and progestogens with a predominance of the latter, refers to new generation drugs. In case of reception according to the instructions and without gaps - a soft option with maximum reliability.
Non-hormonal contraceptives
Spermicides (Benatex, Conratex, Traceptin) work locally, so this contraception is used only before intercourse and additionally plays the role of protection against pathogenic microorganisms. Non-hormonal contraceptives have few side effects and contraindications, which gives them an advantage over taking oral drugs. However, they cannot be used daily, and among the significant disadvantages - they cause irritation of the vaginal mucosa.

Birth control after intercourse
Doctors distinguish emergency contraception as a separate category, which should not be resorted to often: these are not the best, but strong medicines that cause damage to health and the reproductive system. There are 2 options:
- Preparations on levonorgestrel (Escapel, Microlute) - these contraceptives are taken within 24 hours after sexual intercourse: 1 tablet immediately and another 1 tablet 12 hours later.
- Medicine on mifepristone (Zhenale, Mifolian) should be drunk within 72 hours after sexual intercourse.
Mechanism of action of oral contraceptives
The key difference between medicines that need to be taken orally and vaginal ones is the effect on the hormonal background of the whole organism, and not on the vaginal microflora. Oral contraception is distinguished for good performance when comparing effectiveness with local, because:
- Non-combination and combined oral contraceptives change the thickness of the cervical mucus in the cervix, which prevents the movement of sperm, and thin the endometrium.
- The high content of sex hormones in combined oral medicines blocks ovulation, preventing the egg from maturing.
How to choose birth control pills
You need to entrust the task of choosing contraceptives to a specialist: only after consulting a gynecologist, ultrasound of the pelvic organs, examining the mammary glands and passing a detailed analysis (blood from a vein), you can approach the choice of contraceptives. Even the best contraceptives can be dangerous, so don't neglect your doctor's visit and don't try to find them yourself.
Drugs of choice
The best oral contraceptives are as safe as possible, but with close to 100% efficiency. They are selected individually, after a month of admission, the doctor evaluates the result and decides to extend the course or adjust it. Possible options:
- With a not too active sexual life, doctors advise stopping at non-hormonal contraceptives based on nonoxynol (Enkea, Pharmatex).
- For a sensitive organism, single-phase tablets of a new generation (Novinet, Jess) are desirable, which contain estrogen in small quantities (up to 20 mcg) - they cause less harm to the hormonal background.
- For women aged 27 years or more (especially before menopause), gynecologists recommend drinking combined hormonal three-phase contraceptives (Tri-regol, Triquilar).

Contraceptives for hormonal disorders
If a woman began to suddenly appear overweight, accompanied by friability, there is swelling, several menstrual cycles have passed off schedule, the doctor may prescribe microdosed drugs with a contraceptive effect, but first of all, you will need to take tests to find out which indicators need to be regulated. Only combined hormonal pills can act as a medicine: Marvelon, Jess, etc.
Effective pills for gynecological diseases
Some of the contraceptives can have not only a contraceptive effect, but also contribute to the treatment of uterine fibroids, cervical pathologies, and endometriosis. It is possible to prevent ovarian cancer, polyposis. For this purpose, the use of combined preparations is mainly recommended, the course of which is adjusted by the gynecologist every 8 weeks. Possible appointment:
- Minisiston 20 fem;
- Lindinet-30.
How to take birth control pills
The classic COC blister contains 21 tablets (pellets), which implies a course of 3 weeks, followed by a 7-day break. The only exceptions will be some three-phase preparations, where there are 28 tablets. There are several admission rules:
- Drink contraceptives according to the schedule: once a day at the selected hour (i.e., the interval is exactly 24 hours).
- If a medicine has been missed, take it as soon as possible.
- Do not pay attention to menstruation: from the 29th day open a new package.
Side effects and contraindications
Most of the negative reactions to contraceptives are observed from the digestive system (nausea, vomiting), can be expressed in migraine, weight gain. The list of contraindications is determined by which birth control you choose - even the best ones have a long list. Precisely, doctors advise to refuse the use of contraceptives for those who have:
- thrombosis;
- liver failure;
- hepatitis;
- tumors;
- diabetes;
- abuse of nicotine.
The best birth control pills
- Jess - refer to monophasic contraceptives. Among the benefits of these popular pills is a low dose of estrogen (20 micrograms versus 30 micrograms), which makes them safer for women's health, while contraceptive effectiveness is not affected. According to reviews, adverse reactions to Jess and Jess Plus are rare. The principle of admission is “24 + 4”: a smaller amount is placebo tablets, the rest are active. The main disadvantage is the price per package - 1100 rubles.
- Novinet. These contraceptives are similar to Jess: the latest generation of pills with a small dose of estrogen (20 micrograms), but the additional component is desogestrel. The course of admission is 21 days, preferably from the 3rd day of the cycle. After the course you need a week break. Among the good points is the fact that the drug is inexpensive - 490 rubles. for 21 tablets.

- Jeanine is also a representative of single-phase contraceptives, in which estrogen is observed in minimal doses, but higher than that of Jess: 30 mcg. Additionally introduced antiandrogenic component dienogest. Reception schedule - the classic "21 + 7". Among the disadvantages - a large number of adverse reactions. The cost of packaging for the course is 1000 rubles.
- Regulon - belongs to the number of monophasic contraceptives of the budget category (package price - 490 rubles), taken according to the traditional "21 + 7" scheme. The composition is the same as that of Novinet: estrogen + desogestrel, but the first one is 30 mcg, which increases the likelihood of adverse reactions in a woman.
- Yarina. Among the good contraceptive drugs, according to doctors, are Yarina's contraceptives of the combined type, working on estrogen and drospirenone (30 mcg and 3 mg). Gynecologists also prescribe them to eliminate fluid retention (which provokes weight gain) in violation of estrogen levels. The course of admission is standard. Minus - a large number of side effects. Price - from 1100 rubles.
- Logest. These combined contraceptives, working on estrogen (20 mcg) and gestodene, have received a lot of good reviews: some women drink them for more than 10 years and confirm that there were no unwanted pregnancies with them. You need to drink according to the classical scheme - 3 weeks of admission and a week break. The package price for the course is 800 rubles.
- Qlaira is a classic example of estrogen-dienogest combined contraceptives that suppress ovulation. The package contains 4 types of active tablets and 1 placebo. Reception is strictly according to the scheme, where in a certain order the tablets (they differ in color) alternate. A significant disadvantage is the frequent adverse reactions, including problems with menstruation, if long-term use is practiced. The cost of packaging is 1200 rubles.
- Midian. According to women and gynecologists, this contraceptive is an absolute analogue of Yarina, only cheaper (600-700 rubles). The composition is identical, instructions, indications and contraindications too. In terms of side effects, especially after cancellation, the situation is similar, which is the minus of these pills.
- Ovidon is not the most popular variant of hormonal contraceptives, which differs from those described above by a large amount of estrogen: 50 mcg. He supplemented with levonorgestrel. According to gynecologists, these are very effective birth control pills that suppress ovulation, but they are recommended for women who have already given birth and are close to menopause. Active reception - 28 days. The risk of adverse reactions is high due to the considerable dose of estrogen. Budget price - 390 rubles.
- Non-ovlon is close in amount of estrogen to Ovidon (also 50 mcg), but the second component is norethisterone acetate. Reception from 5 to 25 days of the menstrual cycle, a standard break, lasts a week. The risks of a negative response from the body are high, but in terms of reliability, these COCs are in the lead. It is difficult to find in pharmacies, so there is no information on the price.
Pros and cons of taking birth control pills
Hormonal contraceptives help to even out the menstrual cycle, improve the condition of the skin and hair, and prevent some diseases of the reproductive system. However, among the pluses there are also minuses:
- A large number of adverse reactions.
- Possible ovarian cysts.
- Unplanned bleeding.
- Delayed ovulation after withdrawal for 3-6 months.
Oral contraceptives partially or completely suppress ovulation, which prevents pregnancy. Tablets are reliable, they are convenient to take, but due to the content of hormones, drugs can be hazardous to health.
Oral contraceptives help protect yourself from unwanted pregnancy
How to choose contraceptive drugs?
It is better to entrust the choice of oral female contraceptives to a specialist, the doctor will determine the phenotype of the woman, prescribe an analysis to determine the level of sugar, hormonal levels, mammography, ultrasound of the pelvic organs.
Estrogen phenotype
Women of short or medium height, with medium or large mammary glands, deep voice, dry skin, lean hair. The duration of the female cycle is more than 28 days, the duration of menstruation is 5–7 days. PMS manifests itself in the form of nervousness, the chest becomes dense, painful. This phenotype is characterized by abundant discharge of leucorrhoea, but pregnancy proceeds without any special symptoms or complications.
It is better for such women to choose drugs with a large amount of progestogen - Rigevidon, Minisiston.
progesterone phenotype
Women are tall, angular physique, they have a deep voice, small mammary glands, skin and hair are oily, acne often appears. The menstrual cycle is short, menstruation lasts 3-4 days, but the discharge is plentiful. PMS manifests itself in the form of depressive states, lower back pain. There is little leucorrhoea, pregnancy is accompanied by a significant weight gain.
Women of the progesterone phenotype are distinguished by severe toxicosis during pregnancy.
Oral contraceptives should have an antiandrogenic effect - Yarina, Janine, Jess.
Balanced phenotype
For representatives of the mixed type, the characters are feminine forms, medium height, medium-sized breasts, skin and hair of a normal type. The duration of the cycle is 28 days, the duration of menstruation is 5 days, the manifestations of PMS are practically absent, whites are moderate. Pregnancy proceeds normally, without any special complications.
Suitable birth control pills - Novinet, Regulon.
Classification of oral contraception
All contraceptive pills are divided into 2 large groups - mini-pills and combined oral contraceptives, they also differ in the amount of hormones.
Types of oral contraceptives:
- Microdosed- with a minimum content of hormones, they are prescribed to nulliparous women, girls who are taking birth control pills for the first time, or those over 35. The pills have practically no contraindications, they have a pronounced cosmetic effect.
- Low dose- suitable for women who have given birth, can be taken 1.5 months after childbirth to prevent re-pregnancy. Tablets are also prescribed if spotting occurs when taking microdoses. Contraceptives prevent the growth of unwanted hair, the appearance of acne, and have a beneficial effect on the condition of the skin.
- Highly dosed- drugs with a high content of hormones are more often prescribed as therapeutic drugs for hormonal disorders, endometriosis.
Tablets must be taken at the same time, if this rule is regularly violated, condoms must be additionally used, since the effectiveness of oral contraceptives decreases with irregular use.
Mini-pill and COC - what is the difference?
Mini-pills are the easiest contraceptives, they are safe, have a small number of contraindications and side effects, contain only progestogen. The drugs affect the consistency of the vaginal mucus, making it viscous and dense, which prevents the penetration of spermatozoa into the fallopian tubes. With regular intake of pills, the conditions for fixing a fertilized egg worsen, in 50% of women ovulation does not occur at all. Progestin drugs are prescribed for uterine myoma, adenomyosis, endometriosis.
The action of the minipill is based on creating obstacles for the penetration of spermatozoa into the fallopian tubes.
All combined contraceptives contain the same dose of progesterone - this hormone prevents the onset of ovulation, the tablets differ only in the content of estrogen.
COC classification:
- monophasic drugs - contain an equal ratio of estrogen and progestogen;
- biphasic - the dose of progestogen changes twice, depending on the period of the monthly cycle;
- three-phase tablets - the content of the progestogen changes 3 times, depending on the phase of the cycle.
It is necessary to start taking contraceptives from the first day of menstruation, or on the day of a medical abortion. They will begin to act in 14 days, so for 2 weeks you need to use additional contraceptives.
List of the best oral contraceptives
When choosing birth control pills, you need to take into account age, the presence of children, the phenotype, read the instructions before taking it, study the contraindications and possible adverse reactions.
mini pili
Mini-pills belong to the group of progestogens, each tablet contains desogestrel or linestrenol. Means are best suited for lactating women, or if it is impossible to take estrogens, tablets prevent the release of an egg from, change the consistency of cervical secretions, and are considered relatively harmless and gentle.
Oral contraceptives are taken from the first day of the cycle daily
List of the best pills
Contraindications:
- thrombosis, problems with cerebral circulation, angina pectoris;
- hormone-dependent malignant neoplasms;
- severe forms of hypertension;
- serious pathology of the liver;
- allergy to soy, peanuts, lactose.
The package contains 28 tablets, you need to take them without interruption. You need to start taking it from the first day of the cycle, if a woman starts drinking pills from 2 to 5 days, then you need to use barrier contraceptives for a week.
With the right choice of oral contraceptives, spotting in the middle of the cycle should stop after a maximum of 3 months.
Combined preparation with a low content of hormones, the composition contains gestodene and ethinyl estradiol, contraceptive pills. It has an estrogen-gestagenic effect, the mechanism of action is based on the suppression of the production of hormones that are necessary for the maturation of the egg, changes in the secretion of vaginal secretions. Price - 860–880 rubles.
Femoden changes the secretion of vaginal secretions
Tablets are prescribed to prevent conception, normalize the cycle, to reduce heavy bleeding.
Contraindications:
- the presence in the anamnesis of liver tumors, severe forms of pancreatitis, thromboembolism;
- diabetes mellitus with vascular complications;
- migraine;
- uterine bleeding of unknown origin.
Take 1 tablet daily from the first day of the cycle for 3 weeks, take a seven-day break, continue taking the drug, even if menstruation has not yet ended. The contraceptive effect of the drug is preserved if the errors in taking the pills are less than 12 hours.
All birth control pills should not be drunk with an established or suspected pregnancy, uterine bleeding of unknown origin.
Combined monophasic contraceptive, contains drospirenone and ethinylestradiol, 28 tablets in a blister. Price - 1170-1200 rubles.
Jess is intended not only for contraception, but also for the treatment of severe manifestations of PMS
A drug with an antiandrogenic effect, improves skin condition, normalizes the cycle, reduces the pain of menstruation, bleeding becomes less abundant, reduces the risk of developing malignant tumors of the endometrium and ovaries. Drospirenone prevents weight gain, the appearance of edema, reduces the manifestation of PMS.
Jess is intended for contraception, sometimes it is prescribed for the treatment of acne, the elimination of severe symptoms of PMS.
Contraindications:
- thrombosis, thromboembolism;
- migraine, diabetes, vascular pathologies;
- pancreatitis, severe hepatic, renal pathologies, diseases of the adrenal glands;
- malignant tumors.
Start drinking tablets from the 1st day of the cycle, it is possible to start taking them on the 2nd-5th day using additional contraceptives during the week. Take the medicine with meringue break, start a new package immediately after the end of the previous blister.
Cheap pills contain ethinyl estradiol and levonorgestrel, they are three-phase contraceptives. The action of the drug is aimed at suppressing the synthesis of gonadotropic hormones - the rate of egg maturation decreases, ovulation does not occur. Tri-regol is prescribed for contraception and normalization of the cycle. Price - 310-330 rubles.
Tri-regol is the most affordable version of the pills that prevent the maturation of the egg.
Contraindications:
- age over 40;
- lactation;
- jaundice;
- thrombosis, thromboembolism;
- severe course of diabetes;
- failures in lipid metabolism;
- diseases of the gallbladder, liver, chronic colitis, cardiovascular system;
- migraine;
- some forms of anemia;
- otosclerosis with hearing impairment;
- recent transactions;
- lactose intolerance.
Take 1 tablet daily for 21 days, take a break for a week, after 2-3 days, menstruation should begin. The next package should be started strictly after 7 days, even if menstrual bleeding has not yet ended.
Combined contraceptives containing dienogest and ethinylestradiol, monophasic contraceptive pills with antiandrogenic action. Jeanine is prescribed to prevent unwanted pregnancy, normalize the cycle, reduce the pain of menstruation and the amount of discharge, with acne, androgenetic seborrhea and alopecia. Price - 1.1-1.2 thousand rubles.
Jeanine is a monophasic drug to prevent unwanted pregnancy.
Contraindications:
- vascular pathologies, thrombosis;
- serious liver disease;
- malignant neoplasms.
Take 1 tablet from the first day of the cycle for 3 weeks, take a week break, continue taking the drug, even if menstruation has not yet ended.
The latest generation drug based on drospirenone and ethinylestradiol, refers to monophasic low-dose oral contraceptives, the drug suppresses the onset of ovulation, increases the viscosity of the uterine cervical secret. During the reception, the cycle normalizes, menstruation becomes less painful, the amount of discharge decreases, while extra pounds do not appear, there are no edema. Price - 1.2–1.3 thousand rubles.
Yarina is a monophasic low-dose drug of the latest generation
Contraindications:
- stroke, heart attack, angina pectoris, ischemic attacks, tendency to form blood clots;
- pancreatitis current or in history;
- diabetes with vascular complications;
- atrial fibrillation, hypertension, smoking after 35 years, vascular pathologies of the heart and brain;
- severe diseases of the kidneys, liver;
- malignant neoplasms;
- breastfeeding period.
Take 1 tablet for 3 weeks, you need to drink the medicine from the next package after a week break. When switching from another contraceptive to Yarina, the scheme does not change - you need to drink new pills the next day after the old one, if the blister contains 28 pills, or after a standard seven-day break.
Low-dose monophasic drug with antiandrogenic and contraceptive effect, eliminates the manifestations of acne and seborrhea, 21 tablets per pack. Price - 700 rubles.
Siluet, in addition to the contraceptive effect, eliminates the manifestations of acne
Contraindications:
- thrombophlebitis, thrombosis;
- ischemia, angina pectoris;
- pancreatitis, jaundice, liver pathology;
- hypertension;
- vascular complications that arose against the background of diabetes mellitus;
- epilepsy;
- lactation.
Take 1 tablet per day in the order indicated on the blister for 3 weeks, start taking the next pack after a seven-day break.
An inexpensive but effective low-dose monophasic contraceptive based on levonorgestrel and ethinyl estradiol. With regular intake of tablets, the cycle is normalized, the risk of neoplasms is reduced, the drug is prescribed for severe PMS, dysmenorrhea. Price - 480-500 rubles.
Minisiston is an inexpensive contraceptive that normalizes the cycle and reduces the risk of neoplasms.
Contraindications:
- liver tumors, other malignant neoplasms;
- thromboembolism, heart disease;
- severe diabetes mellitus;
- jaundice idiopathic;
- otosclerosis;
- age over 40 years.
Take 1 tablet once a day from the first day of the cycle for 3 weeks. Then you need to take a seven-day break.
Reliable microdosed three-phase oral contraceptive containing dienogest and estradiol valerate, each package contains 4 types of tablets with different hormone ratios and 2 inactive tablets. The drug is prescribed to prevent pregnancy, reduce the intensity of the manifestation of PMS, treat heavy and heavy menstrual bleeding. Price - 1.2 thousand rubles.
Qlaira is a reliable three-phase remedy with a different ratio of hormones
Contraindications:
- lactation;
- venous thromboembolism, blood diseases;
- a history of more than 2 factors for the formation of blood clots - a genetic predisposition, smoking, obesity, a sedentary lifestyle;
- sore throat, valvular disorders, history of heart attack or stroke;
- drops in blood pressure;
- severe forms of diabetes;
- mammary cancer;
- liver cancer, hepatitis, impaired bile outflow, gallstones.
Take 1 tablet, you do not need to chew, drink plenty of water, with a break between doses of up to 12 hours, a high contraceptive effect is maintained, you need to drink the medicine without a break.
A good microdosed monophasic oral contraceptive containing nomegestrol and estradiol, in a package of 24 active and 4 placebo tablets, prescribed to prevent conception. Price - 1.2–1.3 thousand rubles.
Zoely is a microdosed monophasic drug to prevent conception.
Contraindications:
- thrombosis, thromboembolism;
- migraines of a neurological nature;
- angina pectoris, ischemic attacks;
- diabetes, severe form of hypertension;
- pancreatitis;
- severe liver pathology;
- malignant hormone-dependent tumors;
- lactation;
- lactose intolerance.
Take the tablets in the sequence indicated on the blister, 1 piece per day for 28 days.
Microdosed drug, contains ethinylestradiol, desogestrel, has an estrogen-progestogenic, contraceptive effect, 21 tablets per pack. With prolonged use, the skin condition improves, blood loss during menstruation is reduced, the cycle becomes regular. Price - 500-520 rubles.
With the regular intake of Novinet tablets, blood loss is reduced during the munch, and the cycle becomes regular.
Contraindications:
- lactation, age over 35;
- thromboembolism, thrombosis or the presence of precursors of the development of diseases;
- migraine with signs of neurological disorders;
- diabetes with complications in the form of vascular pathologies;
- pancreatitis, liver dysfunction;
- identified or confirmed hormone-dependent neoplasms;
- otosclerosis;
- smoking.
You need to start taking the drug no later than the 5th day of the menstrual cycle for 3 full weeks, a break from the 22nd to the 28th day, from the 29th day you should start taking the pills from the new package.
A high-dose three-phase drug containing levonorgestrel and ethinyl estradiol, prescribed as a contraceptive, or for correcting the menstrual cycle, in a package of 21 tablets. Price - 750 rubles.
Triquilar is a high-dose drug that will help correct the menstrual cycle.
Contraindications:
- increased risk of blood clots;
- neurological migraine;
- severe forms of diabetes, pancreatitis, liver diseases;
- extensive injuries, surgical interventions;
- malignant tumors, suspicion of their presence.
How to use? The sequence of taking the tablets is indicated on the package, you need to drink them 1 piece per day for 21 days, then take a week break. The tool works, even during a break.
Harm of oral contraceptives
Modern oral contraceptives reliably protect women from unwanted pregnancy, improve the appearance of the skin, and with regular use of pills, the risk of developing cancer of the breast, uterus, and ovaries is reduced. But, despite the large number of advantages, contraceptives have side effects, they cannot be called absolutely safe for health.
Consequences of taking hormonal contraception:
- migraine, depression;
- early alopecia, the appearance of age spots;
- the development of diabetes mellitus, osteoporosis, thrombophlebitis, the risk of stroke increases;
- with prolonged use, the functions of the reproductive organs are disrupted, the structure of the endometrium changes;
- when taking pills for more than 3 years, the risk of developing glaucoma increases;
- if you drink oral contraceptives for more than 5 years, Crohn's disease, multiple sclerosis, venous insufficiency may develop;
- decreased libido;
- deficiency of vitamins B2, B6, the process of absorption of folic acid is disturbed.
Contraceptive pills without side effects do not exist, in order to minimize the harm of hormonal drugs, you need to take regular breaks during the reception, give the body the opportunity to relax. To avoid conception, you can use non-hormonal contraceptives immediately before the act - Pharmatex, Pantex Oval, which are intended for intravaginal administration. The risk of severe consequences, weight gain increases in women who smoke, hypertensive patients, with the wrong choice of pills, the doctor should determine the timing of use.
Contraceptive pills can also be taken with irregular sexual relations - the drugs help normalize the cycle, eliminate the manifestations of PMS, but do not protect against sexually transmitted diseases. If necessary, fertile functions are restored within 2-6 cycles after contraception has been discontinued.
Contraceptives of the new generation rarely cause the development of serious side effects, provided that they are used correctly, but the list of contraindications is quite large. Before starting the use of oral contraceptives, it is necessary to do a comprehensive examination.
 Does ureaplasma pass by itself (can it pass on its own)?
Does ureaplasma pass by itself (can it pass on its own)? PCR analysis to detect chlamydia Chlamydia PCR how to do
PCR analysis to detect chlamydia Chlamydia PCR how to do COCs with different daily dosages: how to choose, an overview of the best drugs
COCs with different daily dosages: how to choose, an overview of the best drugs Ureaplasma parvum: characteristics, tests, symptoms in women and men, what is dangerous, whether it is necessary to treat
Ureaplasma parvum: characteristics, tests, symptoms in women and men, what is dangerous, whether it is necessary to treat Basic technologies for obtaining nanomaterials
Basic technologies for obtaining nanomaterials How to tell the time in English?
How to tell the time in English?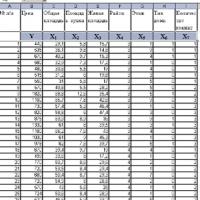 Introduction to Multivariate Statistical Analysis
Introduction to Multivariate Statistical Analysis